I was *just* getting used to my new self...
I am a 43 year old BC survivor, ER/PR+, HER2- and I am 3 years out from dx. I chose a bilateral mastectomy, reconstruction, 8 rounds of chemo and have been on Tamoxifen for 2.5 year (only 7.5 more to go! *insert eye roll here*). I had not had a period since right after my 1st chemo treatment in March of 2015 and then on New Year's Day of this year, I had (what I thought was) a period. After over-thinking it, I called my gyn, as a precaution since it had been so long since I had had one. On top of this, my hormones are so wacky, I have gone from "normal" levels, to menopausal levels, then back to normal, more times than I can count in 3 years. I have been dealing with it for so long that I could probably tell them & get within 10 pts of whatever the measurement is they use to measure the hormones based on how I am feeling. I go from hot flashes, short tempered and angry to feeling like a teenager with the erratic libido and a side of acne. ALL of this has become normal to me and I literally have just started becoming more comfortable/confident as my "new self"!
Of course you know that as a cancer survivor, if you sneeze wrong, they want to scan you. Although I am grateful for the attentive care from my medical team, it has become so annoying that I have to spend time still in the dr office (and MONEY! HELLO, January and a new deductible!). Regardless, my gyn said I should go for a pelvic ultrasound. I (reluctantly) did, in January. The report showed endometrial hyperplasia, a cyst on the left ovary and a "unremarkable" rt ovary (how rude to talk about my ovaries like that, right? LOL, in all seriousness, can that just say she looks "healthy" and not use such a negative description?). They stated I should follow-up in March, which I did. The cyst on the left ovary had gotten smaller, the endometrial lining was still thick. I was focused on the cyst and felt like I should go home and celebrate.
After dealing with some "challenging" clinic staff at my gyn office, I was told to come in for a uterine biopsy. I (reluctantly) did. I asked her if I was doing the biopsy b/c 1)I had a thickened uterine lining or 2) b/c the lining was thicker from January to March; she stated it was the latter, that Jan it measured 9mm, March 14mm. When I asked her what it should measure, she stated that it depends on if I am menopausal. My response was, "well, today I am!". She said menopausal women should be under 5mm. On top of this fantastic news, literally during the biopsy, the dr stated that she didn't feel like she got a "good sample" but she "didn't want to torture me any more", so she sent it off as is. The results came back as non-malignant. Again, I thought I should celebrate! When I spoke to her MA to discuss the pathology results, I asked if it non-malignant b/c 1)everything looks good, enjoy your life OR 2)the sample was too small....her (the Medical Asst) response: "WELL, THE SAMPLE THAT WAS SENT WAS NON MALIGNANT.....BUT THERE COULD BE CANCER SOMEWHERE ELSE". Umm....excuse me?!?
OK, moving on....I actually went INTO the dr office, WITH my husband to get this all straightened out. Let me just throw in (if you're still reading this long post) that I LOVE my gyn....I do not like her office, or the staff. So, I suck it up b/c I think she is pretty fantastic, plus she works really well with my Oncologist, and vice-a-versa. So, my gyn says I should either do a D&C or a consider a hysterectomy. I asked her why I would choose the D&C over the hysterectomy and she responds, "to avoid having the hysterectomy, which even though they're both done in the hospital, the hysterectomy is more invasive". My response was, "am I avoiding a hysterectomy by doing a D&C? Or...just postponing it?" Her response was that I was most likely postponing it, that I "my ovaries aren't doing much anyway" and I "have hormones that have already tried to kill me once" and that if it were her, she would get it all out. So...I have a hysterectomy scheduled for April 25.
OK...the whole point of my post is this: I am not scared of the surgery (heck, I am looking forward to the chemically-induced nap!), I am not scared of the recovery (can it really be worse than a bilateral mastectomy? At least I won't have drains this time!). I am so scared of how I am going to feel 6 months, or 12 months down the line, after permanently removing my struggling lady bits (ie: my ovaries along with my uterus, cervix and fallopian tubes). One of the things I didn't really consider when deciding about cancer treatment is how I would feel AFTER the treatment. I just wanted to get through it, get my hair back, and everything would be la-de-da. I was mistaken. But I have come to accept that. And I am trying to learn from my past experiences. And even though I don't think I made a mistake with the treatment I chose 3 years ago, I just want to make sure I am not going to be some dried up, crusty old version of myself, rocking myself in the corner b/c I can't take any HRT. Ever.
I go from feeling like I am so grateful that I am in tune to my body and I got this random period checked out, because otherwise, how would anyone know I had a thickened uterine lining? And then I swing 180 degrees (kind of like my wonky hormones) and think that this has just gotten blown WAY out of proportion. I know that Tamoxifen can cause the uterine lining to thicken, mine might be b/c of that, or b/c I have 3 year's worth of lining since I haven't had a period. I know that it is all probably a ticking time bomb and I should just get it out. My gyn says that she tells all of her patients that are on Tamoxifen and dealing w/ a hysterectomy that *we* shouldn't feel any WORSE than how we've felt on Tamoxifen. Well, I haven't felt terrible! I mean, I don't like it, I've gained a little weight, my skin is crazy dry and I feel like I look like I've aged 10 years in the last 2...but the devil you know is better than the devil you don't, right? And now, I'll have to be off of the Tamoxifen and get on something different, since I will get the official badge of menopause. That scares me, too! What if that rx is worse?
Let me just say "Thank You" to those of you that have stuck through my long post and read to here. If anyone has any experience similar to mine, I would be grateful for any tips or advice.
Comments
-
Dblomom,
Oh do I ever know what you're saying! I was on tamoxifen for about 5 minutes when the trouble started (exaggerating of course, I was approx. 5 months on it) when the bleeding started, on and off for months. After having polyps removed in the gyn office (OUCH, I'd rather have had root canal) on two occasions, 2 hysterosonograms, (double OUCH) failed uterine biopsy (scant tissue) and my thickness up to 17 mm (YIKES) it was recommended I go for the D&C (I called it my 'dry cleaning') My MO & GYN wanted to see results before proceeding to a hysterectomy. The results came back negative for cancer and I haven't had any problems/bleeding/polyps in the last 3.5 years. For me personally, I'm glad I made the decision to go this route, although I have to be vigilant if bleeding should start again. My thickness is now steady at 4 mm. If the bleeding starts again (please god no!) I'd do the same as I'm confident in my doctors. I'm also up for the switchover to an AL in December so the tamoxifen induced thickening of the lining shouldn't be as much of a concern (please god, again!) The decision is such a personal one, so in no way am I advising you which way to go. The AL's have their own set of problems as does tamoxifen. What I have learned here is that if the side effects are debilitating you can switch back or switch types (good news for me). I plan on sucking it up, hopefully. I hear you when you say "just getting used to the new me". It seems like a new curveball gets thrown at us just as we get comfy. I guess its another opportunity to make a new and improved 'new me' from time to time. For Christmas I want a 5 year moratorium on change lol!
Sending lots of positives your way in your decision making, hope it goes smoothly for you whatever you decide. Keep us posted please!
-
(1) I won't be of much actual help to you.
(2) But I love your attitude!
(3) I know several women who have had hysterectomies without the oophorectomy. I think I read <most of> your post. Is that an option?
(4) IF IT WERE ME (huge "if"), I'd consider the D&C. It might be kinda like why I've opted for lumpectomies rather than MXs. I tend to be conservative in treatment and I guess I'm not seeing a terrible downside to not doing the hysterectomy at this point? Or am I missing something?
-
The good news is that you can still take Tamoxifen, and have the hysterectomy//oopherectomy. It was the easiest surgery and recovery was a snap. The lumpectomy was more difficult for me. I feel great, I don't worry about reproductive issues/continual cycles. The fear of the what iffs is gone, baby gone. I take Tamoxifen because I have early stage osteopenia and do not want further bone thinning from AI's. I have found Tamoxifen very doable.
If there is every any problem, I like the idea of eliminating problems with uterus and ovaries.
I use heavy duty moisturizers, such as vaseline, serious skincare vitamin c crepe resist, etc. Also, I like to layer product on my hair to keep the moisture in.
My surgery was Jan 17 and I do not regret it, at all.
-
I’m 44, had bmx w/DIEP recon, and tamoxifen. I had awful joint pain and terrible brain fog, hot flashes, acne acne and more acne on tamoxifen plus I was allergic-severe itching on it. Developed blood clots and discontinued tamoxifen. Genetic testing cane back positive for an ovarian cancer gene. Had ooph/hyst done using the lap/vag technique. Easy surgery. I kept asking if they were sure they did it because it didn’t hurt at all. Started letrozole/femara (AI). hot flashes returned, brain fog is gone but I lose train of thought easy, and my thumb and pointer finger hurt in the mornings when I wake up. Acne also cleared up. Those are the extent of the side effects from surgery and AI at this point. So overall I’m in a better situation after ooph/hyst + AI. And I’m not a dried up crusty woman in the corner either. Everyone is different, but I’m of the same opinion as your GYN and take it out. Why risk it?
-
I did 2 years on Tamoxifen then needed a hysterectomy due to thickened lining. I was 52 and not yet menopausal. It's now been 3 years and I can honestly say I feel great! I didn't feel any worse after the HX. I figured all the aches and pains were Tamoxifen anyway. I will say I did not have hot flashes until the HX though. When my doc said time to pull the lady bits I panicked just like you. I was so freaked out about how I was going to handle the "aftermath". My wonderful GYN just pointed out that I would handle it just like i did BC....with guns blazing. He reminded me that I would go through it anyway at some point but it might just be a little rougher since it was surgically induced menopause as opposed to "regular". He was right. Surgery was a breeze. I've had teeth cleanings that were rougher. I was walking at day 3, back at the gym at day 12 (albeit just easy walking) and fully functional at 8 weeks. I took Tylenol for the first 3 days then nothing after that. The hardest thing to do was to do nothing! Yes I have hot flashes, yes I can't seem to shake these last 10 pounds but the peace of mind of not having to worry about "that" cancer is awesome. Now, I do still get annual pap smears because as my GYN pointed out " you may not have a uterus, or ovaries or even a cervix but you still have a vagina so you can still get vaginal cancer". And when my best friend called me yesterday ( who had BC last year) crying hysterically cause she had a "suspicious" pap, I realized I really was glad to have done the hysterectomy. And my sister, who is going through menopause now, calls me everyday crying about how dry she is and how she suspects she has vaginal atrophy and keeps getting yeast infections, etc and she's NEVER had a hysterectomy. So just because you get it all removed doesn't necessarily mean it'll be awful. You seem to deal with BC with humor and grace, I feel certain you can deal with a hysterectomy with the same aplomb.

Oh and by the way....I never swapped from Tamoxifen to an AI after my hysterectomy. I finished out my 5 years. My docs all said since I did ok on Tamoxifen why swap to a much worse therapy for only a couple of percentage points improvement in prevention. They said the hysterectomy combined with the Tamoxifen helped as much as an AI would without all the crappy SEs.
And one last thing....those chemically induced naps are delicious aren't they? I'm particularly fond of Propofol. I even requested it for my colonoscopy which I actually looked forward to. Hmmm.....I think BC might have made me an anesthesia addict!
-
@Egads007~I am glad you (and a lot of others) can relate! I was naive 3 years ago in thinking that if I could just navigate through the surgeries, chemo and treatment for BC, it would be smooth sailing for the rest of my years!
@Ingerp~1. you were a ton of help, you actually made me laugh OUT LOUD, which is not an easy task. I loved your response (especially the format). :-D
@Michelle_in_cornland~I think you and I are of the same mindset. I am a HUGE What If-er, I just needed the reminding that this is do-able! And I may give a little push-back to my MO about switching from Tamoxifen after reading these responses. Prior to this, I didn't know it was an option to stay on it (vs. an AI) after menopause. I mean, I am not in love with the rx, but honestly, it hasn't been *that* bad.
@Lula73~I appreciate you sharing your interaction on the AI! It is comforting to hear that. And yeah, when I asked my breast surgeon, who I happened to have an (unrelated)appt with right after we scheduled this surgery, what she thought about it, her response was, "If someone offered me a hysterectomy, I would take it". ;-)
@lala1~THANK YOU for recounting your experience! I have 1 friend who had a similar experience as yours, she said it was the best week of her life. She said, "OMG, it was great, I just laid around and ate narcotics for a week" (she's usually wound very tight and practically lives in her car from toting kids to games/practice/etc). But then I had another friend, who I love dearly, but....she was texting me all of her horror stories! And...coincidentally, we have the same gyn! She even said "make sure the anesthesiologist gives you EVERYTHING they can for nausea, the nausea....it's so bad" and on and on. I finally said (over text), "good grief, what is she going to be doing to make me so nauseous?!?!?" She responded that it is just b/c you are under such deep anesthesia for SO long. I said, "umm...how long is this surgery?!?!". She said, "Oh, like AN HOUR!". I said, "ok.....well, my mastectomy was 6 hours so.....thank you for the *tip*, I should be good to go". I know she meant well but....it's funny, kind of like when you are pregnant and everyone you meet wants to tell you how horrific childbirth is. I can only hope my recovery is as seamless as yours. And, like I said to Michelle_in_cornland, I had no idea that staying on Tamoxifen would even be an option, so thank you for sharing that! Since I haven't really had anything negative side effects, except maybe this uterine thing, maybe I can talk them into letting me ride it out on Tamoxifen. ;-)
Side note~It has been a while since I have gotten on this BC site, even just to read posts....sometimes it is hard to put it all out there, and putting it in writing definitely makes it more real. My sense of humor is sarcasm and sometimes that does NOT translate well via any form of text. So thank you all for your candid, heartfelt, honest responses, for being able to read through my tongue-n-cheek voice and for being able to see a little of who I am through a post. It definitely has eased my mind going into this next chapter. xoxo
-
dblomom, you might want to consider the risks and complications of a hysterectomy before you rush into it.
And there are several different kinds of hysterectomy procedures as well.
More at
https://www.uspharmacist.com/article/complications...
Surgical and Postsurgical Complications
Hysterectomy is generally a safe procedure, but with any major surgery comes the risk of surgical and postsurgical complications. Such complications commonly include infection, hemorrhage, vaginal vault prolapse, and injury to the ureter, bowel, or bladder.6,7Although hysterectomy is associated with fewer complications than many other major operations, risks and complications depend upon the type of hysterectomy performed, the individual woman's health status, and the surgeon's expertise and experience.4,6,7
Infection: Postoperative fever and infection are responsible for the majority of minor complications following hysterectomy. Infection occurs in approximately 6% to 25% of patients who undergo abdominal hysterectomy versus 4% to 10% of those who undergo vaginal hysterectomy. Despite impeccably sterile surgical technique and careful patient selection, women undergoing a hysterectomy procedure have a 30% chance of postoperative febrile infection.2
In both abdominal and vaginal hysterectomy, pelvic infection occurs in approximately 4% of cases.8,9 Pelvic cellulitis is an infection of the soft tissues and usually occurs around the third day following surgery. Although some degree of cuff cellulitis probably occurs following the majority of hysterectomies, antibiotics are not required unless fever persists. Additionally, the rate of postoperative symptomatic urinary tract infection is approximately 1% to 5% in patients who undergo hysterectomy. Immediate catheter removal postoperatively is strongly recommended to reduce the risk of this complication.8-10
Risk of postoperative infection can be lowered substantially with the use of prophylactic antibiotics.8,9 Studies reveal that women who receive prophylactic antibiotics prior to an abdominal or vaginal hysterectomy have a reduced rate of wound infection, pelvic cellulitis, vaginal cuff abscess, and pelvic abscess.9 The proper dosage should be administered 30 minutes prior to surgery to ensure that therapeutic levels are achieved in tissue at the surgical site. Agents such as cefazolin, cefotetan, cefoxitin, metronidazole, and clindamycin have all proved effective.8-10 If postoperative fever persists and infection is suspected or identified, a broad-spectrum intravenous antibiotic covering anticipated pathogens should be initiated. Antibiotics should be continued for 24 to 48 hours after the resolution of fever and symptoms.8,9
Ureteral Injury: Ureteral injury is becoming a more frequent posthysterectomy complication as the number of laparoscopic-assisted procedures increases. The incidence rate of this complication in laparoscopic-aided procedures is 0.7% to 1.7% with abdominal hysterectomy and 0% to 0.1% with vaginal hysterectomy.10 Injuries generally occur with excessive electrocautery and lasering adjacent to the ureter. These injuries are best managed with resection of the damaged portion and reimplantation of the ureter.11 Surgeons should recognize urologic injuries and correct them intraoperatively to avoid serious postoperative complications that occur from urinary extravasation.10,11Bladder Injury: Injury to the bladder occurs in approximately 0.5% to 2% of all hysterectomies. 8,12 Bladder injury most likely occurs during entry to the peritoneum or during dissection of the bladder off the lower uterine segment, cervix, and upper vagina. Several studies have concluded that partial disruption of the innervation of the bladder during hysterectomy may result in postoperative incontinence.13,14 A systematic review reported that hysterectomy was considered a risk factor for urinary incontinence in women older than 60. 14 In another study, urge incontinence was found to be more common than stress incontinence in women posthysterectomy.13 In 2002, a large cohort study revealed that women older than 50 were less likely to have improvement with urinary incontinence after hysterectomy compared to younger women.15
Bowel Injury: Although bowel injury is uncommon, particularly with vaginal hysterectomy, it is a serious complication associated primarily with laparoscopic-assisted abdominal hysterectomy. During both abdominal and vaginal surgery, the rectum and ascending and descending colon can be injured.8 Bowel injuries occur during the lysis of adhesions involving the bowel and dissection of the posterior cul-de-sac. Preoperative bowel preparations will allow for incidental colon surgery without the necessity of colostomy. If a large bowel injury should occur and no preoperative bowel preparation was given, a temporary diverting colostomy may be indicated to protect the suture line and lower the risk of peritonitis and sepsis.10
Hemorrhage: One of the most serious postoperative complications associated with hysterectomy is hemorrhage. Excessive bleeding complicates approximately 1% to 3% of all hysterectomies.12 In most cases, bleeding originates at the lateral vaginal angles and is amenable to vaginal resuturing. Average intraoperative blood loss can range anywhere from 300 to 400 mL.16 Early postoperative signs of hemorrhage after vaginal hysterectomy include bleeding from the vagina, deterioration in vital signs, decreased hematocrit level, and flank abdominal pain.
It is routine to cross-match blood in patients undergoing hysterectomy. Two to four units of packed red blood cells should be available at all times. Women who are more likely to need blood transfusion include those undergoing peripartum hysterectomy or hysterectomy for gynecologic cancer, as well as those undergoing elective hysterectomy with pelvic inflammatory disease, or pelvic abscesses or adhesions.10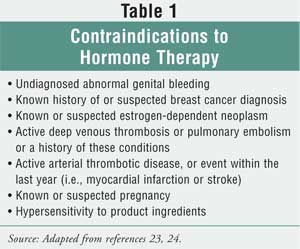
Thromboembolic Disease: The risk of venous thromboembolism following abdominal hysterectomy in low- and high-risk patients is 0.2% and 2.4%, respectively.9,10 The risk of deep venous thrombosis and pulmonary embolism can be minimized with the use of graduated compression stockings perioperatively and early ambulation postoperatively. The type of prophylaxis recommended depends upon each patient's risk factors. Risk factors include obesity, malignancy, previous radiation therapy, immobilization, estrogen use, prolonged anesthesia, radical surgery, and personal or family history of thromboembolic disease. Patients at high risk for thromboembolism may be given a low-molecular-weight heparin or 5,000 units of subcutaneous heparin preoperatively and then every eight to 12 hours postoperatively to reduce the risk of thromboembolic events.8-10
Fallopian Tube Prolapse: Fallopian tube prolapse is an uncommon postoperative complication of hysterectomy. A predisposing factor for prolapse is the presence of a hematoma or abscess at the vaginal apex.8,9,11 If the tissue does not respond to conservative treatment, such as cryotherapy or silver nitrate application, a biopsy of the area may be warranted.9 Surgical interventions are recommended for the management of fallopian tube prolapse. 8,9
Vaginal Vault Prolapse: Vaginal vault prolapse is a type of pelvic organ prolapse that can happen following surgical removal of the uterus. It often occurs when the top of the vagina loses the support of the uterus and then sags or drops into the vaginal canal. Most women with vaginal vault prolapse will also have bulging of the small bowel into the vagina, as well as other bladder and bowel problems such as urinary incontinence and constipation.6,7,15,16 It is important to note that vaginal vault prolapse may be treated with a vaginal pessary, a special device that holds the vagina in place; in some cases, surgery may be warranted.16
Vaginal Cuff Evisceration: A rare complication that can occur following a hysterectomy is evisceration of the small intestine into the vagina.7,9,17 It is associated with the Valsalva's maneuver, severe vomiting, or coughing. Symptoms usually include vaginal bleeding or discharge, abdominal-pelvic pain, pressure in the vagina, and protrusion of bowel. Although eviscerations usually occur early in the postoperative period, one study of 12 patients reported occurrence 27 months after various pelvic procedures.17 Medical treatment usually includes administration of intravenous fluids and broad-spectrum antibiotics and immediate laparotomy with replacement of the mesentery and small bowel. 6,7,9
Possible Long-Term Complications
Many of the clinical findings concerning the long-term side effects of hysterectomy are conflicting. Data show some women develop the complication, while others experience relief from the same complication. For example, some studies have shown increases in psychosexual dysfunction after hysterectomy, while others have shown improvements in this area.3,18 Discrepancies in the data make it difficult for clinicians to clearly identify the long-term risks of hysterectomy and for women to determine if the possible benefits of hysterectomy outweigh the risks.Early Menopause: Many of the long-term complications associated with hysterectomy arise secondary to changes in hormonal balance. Bilateral oophorectomy is performed in more than 50% of hysterectomies in the U.S. and is controversial.1 Some practitioners believe the ovaries should be removed to prevent future development of malignancy, while others prefer to conserve "normal ovaries" to preserve sex hormone secretion and avoid long-term hormone therapy (HT), especially in women with contraindications to estrogen therapy (Table 1 ).19 When the ovaries are removed, levels of ovarian sex hormones, namely estrogen, progesterone, and testosterone, rapidly decline, resulting in sudden menopause.
Studies have found that even those women who keep one or both ovaries experience menopause at an earlier age. A retrospective trial found that women who had had a hysterectomy with preservation of one or both ovaries experienced menopause an average of 5.5 years earlier than women who had not undergone hysterectomy. In this study, no difference was found between women with one versus both ovaries, though some studies have reported differences.19 It has been theorized that early ovarian failure may occur due to disruptions in ovarian blood flow, which is necessary for proper sex hormone production.19,20
Studies have consistently shown HT to be effective for the reduction of menopausal symptoms.21-24 Common symptoms of menopause include hot flashes, night sweats, vulvar and vaginal atrophy, vaginal dryness, insomnia, and sleep disturbances. Initiating estrogen therapy immediately after hysterectomy with bilateral oophorectomy is important in order to prevent onset of menopausal symptoms, although some practitioners may be hesitant to prescribe long-term HT due to the findings that led to the early termination of the Women's Health Initiative (WHI) trial. 25
In February 2004, the NIH decided to terminate the WHI estrogen-only trial before its proposed March 2005 end. Because this trial failed to show that estrogen protects women from coronary heart disease and demonstrated statistically significant increases in the incidence of stroke and deep venous thrombosis, the NIH deemed it unacceptable to subject healthy women to these risks and therefore stopped the trial early. It is important to note that the WHI estrogen-only trial did find a significant reduction in hip and other fractures, as well as an unexpected decrease in breast cancer incidence (P = .06). The WHI trial also demonstrated that when estrogen replacement therapy (ERT) is used for the treatment of menopausal symptoms after hysterectomy, an overall balance of risks and benefits exists, and most importantly, no effect on total mortality was seen throughout the 6.8-year follow-up period.25
Women whose ovaries are preserved should be counseled concerning common menopausal symptoms, and estrogen therapy may be considered when these symptoms are present.19 The duration of ERT after hysterectomy has been debated, and no current guidelines are available to aid practitioners with this treatment decision. Many clinicians are now using ERT through the average age of natural menopause (approximately age 50) and then tapering women off therapy slowly to help prevent reappearance of symptoms.25 If symptoms recur during dose tapering, ERT may need to be restarted or nonhormonal agents may be tried. Nonpharmacologic techniques for treating menopausal symptoms are outlined in Table 2. If a woman simply undergoes oophorectomy and her uterus is preserved, progesterone should be added to the treatment regimen to prevent endometrial hyperplasia.24,26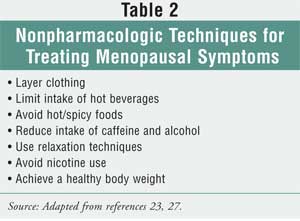
Impaired Sexual Function: Studies have found that concern about posthysterectomy sexual dysfunction is the most common cause of anxiety for women undergoing the procedure.20 There are many plausible mechanisms by which sexual dysfunction may occur, including shortening of the vagina, disruption of innervation of the vagina, and vaginal dryness due to estrogen deficiency.3,20,28,29
Conversely, sexual function may improve posthysterectomy. It has been postulated that sexual function is improved through relief of pain during intercourse due to removal of pelvic pathology, relief of dysmenorrhea, and increased libido due to decreased fear of conception.20
Clinical data are split concerning the true effects of hysterectomy on a woman's sexual function. Early retrospective data found that hysterectomy causes a significant decline in sexual function.3 To the contrary, more current data derived from prospective clinical trials show improvements in sexual function, including increases in frequency of intercourse, sexual desire, and strength and occurrence of orgasms, as well as reductions in dyspareunia.20,28
It was once thought that retaining the cervix would result in less sexual dysfunction due to a decrease in neurologic and anatomic disruption, although clinical trials have not supported this theory.28,29 A 2003 prospective observational study examined the differences between the effects of vaginal, subtotal abdominal, and total abdominal hysterectomy on sexual function and found significant improvements in sexual function with all three types of hysterectomy, with no significant differences among the three types.28
Psychological EffectsData are also mixed concerning the effects of hysterectomy on psychological functioning. As seen with other complications of hysterectomy, retrospective studies have reported adverse psychological outcomes, whereas prospective studies have not supported these claims.3 In fact, prospective studies have shown that hysterectomy improves mood and quality of life in many women by relieving preexisting distressing gynecologic symptoms.3,26
It has been well established that one of the most important influences on postoperative psychiatric morbidity is preoperative psychiatric state.26 Women with psychiatric illness prior to surgery are much less likely to show improvement in this regard after hysterectomy.3,26 Other factors that have been associated with increased risk of emotional distress posthysterectomy include loss of childbearing capacity, adverse effects on a woman's self-image, social disruption due to a long recovery time, and history of inadequately dealing with loss.3,30 The results of a meta-analysis showed that early detection of ovarian failure, immediate initiation of HT in perimenopausal women and in those undergoing oophorectomy, and regular follow-up may improve psychological outcomes of hysterectomy.31
Conclusions
Although hysterectomy is generally a safe procedure, it is pertinent for pharmacists to be aware of the surgical, postsurgical, and long-term complications involved. Educating women concerning the possible complications involved with hysterectomy may ease patients' preoperative anxiety and ultimately improve outcomes. Pharmacists have an important role in the care of this population of women and can aid in the prevention and treatment of complications associated with hysterectomy by providing proper education, identifying high-risk patients, and assisting with the management of medications. -
Thank you for sharing your story. I am going thru a,similar problem with my uterus lining. It has, gone from 15 mm to 23 mm in 3 months and I have cysts on my ovAries thAt are now causing pain. I was,just tested so waiting for my Dr to go over my options. I am so scared of cancer coming back its crazy. I have been on Tamoxifen for 2 years and have every side effect there is. Being a survivor is a non stop anxiety attack sometimes. I am hoping to just have a hysterectomy and just moving on. Praying no Cancer in my lining.
Thanks for letting me vent !
Categories
- All Categories
- 679 Advocacy and Fund-Raising
- 289 Advocacy
- 68 I've Donated to Breastcancer.org in honor of....
- Test
- 322 Walks, Runs and Fundraising Events for Breastcancer.org
- 5.6K Community Connections
- 282 Middle Age 40-60(ish) Years Old With Breast Cancer
- 53 Australians and New Zealanders Affected by Breast Cancer
- 208 Black Women or Men With Breast Cancer
- 684 Canadians Affected by Breast Cancer
- 1.5K Caring for Someone with Breast cancer
- 455 Caring for Someone with Stage IV or Mets
- 260 High Risk of Recurrence or Second Breast Cancer
- 22 International, Non-English Speakers With Breast Cancer
- 16 Latinas/Hispanics With Breast Cancer
- 189 LGBTQA+ With Breast Cancer
- 152 May Their Memory Live On
- 85 Member Matchup & Virtual Support Meetups
- 375 Members by Location
- 291 Older Than 60 Years Old With Breast Cancer
- 177 Singles With Breast Cancer
- 869 Young With Breast Cancer
- 50.4K Connecting With Others Who Have a Similar Diagnosis
- 204 Breast Cancer with Another Diagnosis or Comorbidity
- 4K DCIS (Ductal Carcinoma In Situ)
- 79 DCIS plus HER2-positive Microinvasion
- 529 Genetic Testing
- 2.2K HER2+ (Positive) Breast Cancer
- 1.5K IBC (Inflammatory Breast Cancer)
- 3.4K IDC (Invasive Ductal Carcinoma)
- 1.5K ILC (Invasive Lobular Carcinoma)
- 999 Just Diagnosed With a Recurrence or Metastasis
- 652 LCIS (Lobular Carcinoma In Situ)
- 193 Less Common Types of Breast Cancer
- 252 Male Breast Cancer
- 86 Mixed Type Breast Cancer
- 3.1K Not Diagnosed With a Recurrence or Metastases but Concerned
- 189 Palliative Therapy/Hospice Care
- 488 Second or Third Breast Cancer
- 1.2K Stage I Breast Cancer
- 313 Stage II Breast Cancer
- 3.8K Stage III Breast Cancer
- 2.5K Triple-Negative Breast Cancer
- 13.1K Day-to-Day Matters
- 132 All things COVID-19 or coronavirus
- 87 BCO Free-Cycle: Give or Trade Items Related to Breast Cancer
- 5.9K Clinical Trials, Research News, Podcasts, and Study Results
- 86 Coping with Holidays, Special Days and Anniversaries
- 828 Employment, Insurance, and Other Financial Issues
- 101 Family and Family Planning Matters
- Family Issues for Those Who Have Breast Cancer
- 26 Furry friends
- 1.8K Humor and Games
- 1.6K Mental Health: Because Cancer Doesn't Just Affect Your Breasts
- 706 Recipe Swap for Healthy Living
- 704 Recommend Your Resources
- 171 Sex & Relationship Matters
- 9 The Political Corner
- 874 Working on Your Fitness
- 4.5K Moving On & Finding Inspiration After Breast Cancer
- 394 Bonded by Breast Cancer
- 3.1K Life After Breast Cancer
- 806 Prayers and Spiritual Support
- 285 Who or What Inspires You?
- 28.7K Not Diagnosed But Concerned
- 1K Benign Breast Conditions
- 2.3K High Risk for Breast Cancer
- 18K Not Diagnosed But Worried
- 7.4K Waiting for Test Results
- 603 Site News and Announcements
- 560 Comments, Suggestions, Feature Requests
- 39 Mod Announcements, Breastcancer.org News, Blog Entries, Podcasts
- 4 Survey, Interview and Participant Requests: Need your Help!
- 61.9K Tests, Treatments & Side Effects
- 586 Alternative Medicine
- 255 Bone Health and Bone Loss
- 11.4K Breast Reconstruction
- 7.9K Chemotherapy - Before, During, and After
- 2.7K Complementary and Holistic Medicine and Treatment
- 775 Diagnosed and Waiting for Test Results
- 7.8K Hormonal Therapy - Before, During, and After
- 50 Immunotherapy - Before, During, and After
- 7.4K Just Diagnosed
- 1.4K Living Without Reconstruction After a Mastectomy
- 5.2K Lymphedema
- 3.6K Managing Side Effects of Breast Cancer and Its Treatment
- 591 Pain
- 3.9K Radiation Therapy - Before, During, and After
- 8.4K Surgery - Before, During, and After
- 109 Welcome to Breastcancer.org
- 98 Acknowledging and honoring our Community
- 11 Info & Resources for New Patients & Members From the Team