Hypothyroid medication causing high blood pressure
I started Armour thyroid medication about 2 years ago after being dx as hypothyroid - all the symptoms and TSH level. over 10. I've been tolerating this medication well as my symptoms and lab levels all improved. HOWEVER - my previous perfect blood pressure levels have been slowly increasing to pre-hypertension results.
My GP is very concerned and thinking of starting me on BP meds (he knows I HATE taking meds) - and passed a comment about thyroid medication. I researched it and found that breast cancer patients who had radiation treatments are at risk for developing hypothyroidism. No one else in my family has this condition except me - so I'm guessing because my tumor was high 11:00 position my thyroid got zapped. NEXT - the one of the side effects of thyroid medication is to cause elevated BP. Banging my head on the wall.
So I'm trying to figure out if I can wean myself off OR at least lower the dose which is currently 30mg. These pills are SO TINY that I don't know if I can cut in half and am considering skipping every other day. Has anyone else run into these complications? I don't want to end up taking multiple medications to treat all these side effects of one treatment/drug leading to another medication. I already exercise regular and am very active and eat balanced meals - weight normal BMI range.
Any suggestions? I also read that Armour thyroid was the most balanced thyroid medication over the synthetic drugs which had even worse side effects. So I'm trying to figure out if I can get off thyroid medication. Has anyone succeeded in doing this???
Comments
-
I prefer natural remedies but found Armour Thyroid did not work for me, I have taken Eutirox for 19 years now and never had any side effects, and it has not increased my blood pressure......
-
I pulled my labs for the past 2 years and my latest lab has a borderline high T3 - this is why I'm considering a dose cut. The other thyroid labs are within normal range but I see as my T3 has gone up so has my BP. So wondering about a dose adjustment at least. I've read that people generally take thyroid medication for life but wondered if anyone ever was able to stop or decrease dosage?
-
Cp if you were hypothyroid, getting off your replacement hormone would not be possible.
I found this web page that discussed the effects of T3 on BP. Nice explanation.
Your a good researcher, google keywords "Impact of breast radiation therapy on thyroid" and see what it pulls. I know you know how to play with key words.
I have a thought, will see what I can find...........................
-
Cp this looks like a great article for review, but it costs 31$. Get your doc to pull it.
http://www.cancertreatmentreviews.com/article/S0305-7372(07)00080-1/abstract
The key word phrase I used was "impact of breast irradiation on cardiovascular pressure receptors". It pulled other articles, but I was looking for "pressure receptors" specifically. Pulling some more info BBl In order to explain what I'm thinking, which is way different than thyroid, I have to pull together some info
I thought I might be able to gather some info that would help make this easier to explain, but couldn't. Not that it's not out there, I just couldn't get it.
Radiation doesn't just impact cancer cells. Adjacent tissue is affected too. Over the years the area and depth of radiation beams have been better controlled. But still other tissues can be impacted. My thought with your description of the tumor with radiation in the eleven o'clock position, is that the beam was more central. How much were the heart and great blood vessels in the chest impacted? It would take a bit of study to decipher. It may not be decipherable. The heart and the aortic arch are closer in proximity to the path of your radiation. More than the thyroid.
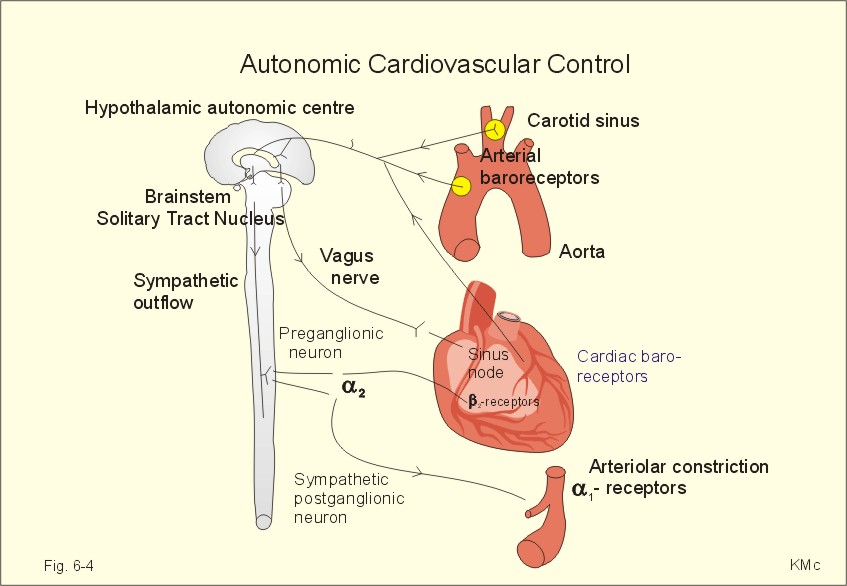
Blood vessels can become stiff b/c of radiation. Scarring. Flow through stiff vessels changes the flow dynamics. Heart cells damaged by radiation can have their ability to respond to an electrical stimulus, and or the ability to contract effectively changed. Plus, if the baroreceptors in the aorta were damaged by the radiation, they may be sending wrong messages to the medulla.
Basic description of normal anatomy: In the aortic arch there are baroreceptors. They're also in the neck and the heart. Baroreceptors measure pressure within the vessel. When the flow dynamics are altered, the baroreceptors sense this and send messages by nerves to the medulla. The medulla sends messages out to the body. The medullas messages are sent through nerves. These messages alter the heart rate, heart force of contraction, peripheral vasculature resistance (more, but enough for now). By changing anyone of these three, the value that we measure as pulse and blood pressure is changed.
The changes in flow dynamics occur every second of every day. This is normal. BUT there are abnormal things that can change the sensing of the baroreceptors i.e plaque. Scarring as with radiation is with in reason as a problem for the baroreceptors, I don't know if it's been studied.
The question that's unanswered is: did your radiation impact the heart or baroreceptors within the aorta?
Hope this is clear?
-
Thanks Sas - yes, I read the first article you listed and have the elevated systolic values pointing to hyperthyroid although I've been treated as hypothyroid. I called the GP office to discuss dropping dose from 30 mg to 15 mg (such a tiny pill to cut in half). This is why I am considering to decrease the Armour dose. Also, I'm still on letrozole which may increase BP for some patients. I've always had excellent BP values until all these treatments and scans which IMO may be the smoking gun. I exercise daily, eat healthy, no drink, never smoked, normal BMI.
I've also been researching MRI contrast dye affect on thyroid as I've been getting a yearly MRI for pancreatic cyst. (Too small to biopsy so GP has 'watched' it.) So far, 5 MRI and the change in my thyroid values coincide with when I started these scans. Maybe the contrast dye instigated these thyroid issues with iodine. I am at the point of refusing these scans with dye - do it without contrast. I am at the 6 year mark and again researched to stop scans after 3-5 years when no change in results.
http://www.medscape.com/viewarticle/820119
http://www.livescience.com/18080-routine-scans-thy...
http://well.blogs.nytimes.com/2012/01/23/iodide-he...
-
I have been taking Armour thyroid for many years (Synthyroid did not work well for me) due to having Hashimoto's Thyroiditis. This is an autoimmune disorder and the most common cause of hypothyroidism (although one's thyroid can certainly be damaged by radiation). It is important to know why you have hypothyroidism and testing can show if it is due to Hashimoto's or not. Many people w Hashimoto's claim they have been able they have been able to quit using or reduce their dependence on thyroid meds by following the Paleo Diet Autoimmune Protocol version-but I'm not disciplined enough to stick w the autoimmune protocol-just straight-up Paleo for me.
I would strongly advise against tinkering with your meds on your own. Reducing your dosage should be done under the supervision of an endocrinologist with careful and frequent monitoring of your thyroid levels. Untreated or under-treated hypothyroidism can lead to increased cholesterol levels and an enlarged/damaged heart, not to mention less dangerous but annoying things like fatigue, dry skin and constipation. Hypothyroidism can also cause low blood pressure (sometimes dangerously low) so taking meds to correct your hypothyroidism can cause your blood pressure to go up.
I have been told if I loose or gain 10 or more pounds my thyroid meds may need to be adjusted. When I started on a Paleo diet 2+ years ago and lost about 25 lbs, I went from taking 120 mg of Armour Thyroid daily to 90 mg (my thyroid doesn't do much on its own, LOL). After loosing weight I felt really good-too good-as in hyperthyroid, causing my endo to reduce my dosage, but this was done with bimonthly monitoring of my bloodwork until we hit the "sweet spot." So I was able to reduce my dosage due to dietary changes/weight loss.
I would also recommend you turn your thyroid treatment over to an endocrinologist rather than a GP if you haven't done so already.
-
CP I just got done revising my post above. Please, reread it now if you will. May seem minor , but it did take a lot of thought to reduce the info to that short post

I've read your post and Labelle's. I agree altering your dose should be done by the doc. I agree that an Endo doc is more knowledgeable than a PCP. But trying to find a doc that will work with you on Armour can be difficult. My local doc wouldn't consider it. But my BIG WIG doc at Moffitt was open to all kinds of variation of drugs. He had an attitude that whatever worked was the route to take.
I had thyroid cancer in 2013-2014. Long story. Based on what I learned in that time it may have been present when I was dx'd in 2009. Papillary thyroid ca is a very slow growing tumor.
I suggest that the minimum level doc that should evaluate the pancreatic cyst is a Gastroenterologist. PCP's aren't qualified. They can read a report from radiology, but the scope of the problem is not within their training.
I haven't got time to read the articles you linked and may not over the next few days. Behind on a bunch of things. Be back
-
Thanks so much for your thoughtful detailed replies. At this time, I really have no idea what triggered my thyroid issues as I had all the antibody screening tests which came back negative. (No family hx either.) I may have been on the edge and then some event/treatment pushed me into the hypothyroid zone. I responded immediately to Armour medication with improved symptoms and labs. I just saw my GP and he mentioned a dose change based on his concerns for my elevated BPs. I called the office today and left a message about decreasing the dose - so he knows this is what I am considering. Previously I had tried looking into an Endocrine specialist but as you mentioned many are opposed to Armour and prefer the synthetic medications. Especially when they heard that I was already taking Armour - they weren't interested in me as a patient. Frankly I don't care to be bullied into a treatment plan if a physician will not discuss and treat me as an individual. I will followup again and see if I can get a referral for one. (For what it's worth, I read some where that Hillary Clinton also takes Armour thyroid medication - don't know if true....)
Regarding the pancreatic cyst (side branch type), when dx I immediately went to NY Presbyterian hospital to a big name GI specialist. He said the standard of care for my situation was to monitor for several years as it was way too small to biopsy. Per patient guidelines they state to monitor with MRI scan 3 times over 5 year period for any change. I've had YEARLY MRI scans (x5) and there has been no changes thank goodness! This is year 6, so I am going for the scan but I am denying the contrast dye. I will only allow if something looks changed. These invasive scans are taking a toll on me.
http://www.gastro.org/info_for_patients/2015/7/27/...
(Also, twice yearly seen by a cardiologist for heart murmur issues - 2 valves affected.)
Categories
- All Categories
- 679 Advocacy and Fund-Raising
- 289 Advocacy
- 68 I've Donated to Breastcancer.org in honor of....
- Test
- 322 Walks, Runs and Fundraising Events for Breastcancer.org
- 5.6K Community Connections
- 282 Middle Age 40-60(ish) Years Old With Breast Cancer
- 53 Australians and New Zealanders Affected by Breast Cancer
- 208 Black Women or Men With Breast Cancer
- 684 Canadians Affected by Breast Cancer
- 1.5K Caring for Someone with Breast cancer
- 455 Caring for Someone with Stage IV or Mets
- 260 High Risk of Recurrence or Second Breast Cancer
- 22 International, Non-English Speakers With Breast Cancer
- 16 Latinas/Hispanics With Breast Cancer
- 189 LGBTQA+ With Breast Cancer
- 152 May Their Memory Live On
- 85 Member Matchup & Virtual Support Meetups
- 375 Members by Location
- 291 Older Than 60 Years Old With Breast Cancer
- 177 Singles With Breast Cancer
- 869 Young With Breast Cancer
- 50.4K Connecting With Others Who Have a Similar Diagnosis
- 204 Breast Cancer with Another Diagnosis or Comorbidity
- 4K DCIS (Ductal Carcinoma In Situ)
- 79 DCIS plus HER2-positive Microinvasion
- 529 Genetic Testing
- 2.2K HER2+ (Positive) Breast Cancer
- 1.5K IBC (Inflammatory Breast Cancer)
- 3.4K IDC (Invasive Ductal Carcinoma)
- 1.5K ILC (Invasive Lobular Carcinoma)
- 999 Just Diagnosed With a Recurrence or Metastasis
- 652 LCIS (Lobular Carcinoma In Situ)
- 193 Less Common Types of Breast Cancer
- 252 Male Breast Cancer
- 86 Mixed Type Breast Cancer
- 3.1K Not Diagnosed With a Recurrence or Metastases but Concerned
- 189 Palliative Therapy/Hospice Care
- 488 Second or Third Breast Cancer
- 1.2K Stage I Breast Cancer
- 313 Stage II Breast Cancer
- 3.8K Stage III Breast Cancer
- 2.5K Triple-Negative Breast Cancer
- 13.1K Day-to-Day Matters
- 132 All things COVID-19 or coronavirus
- 87 BCO Free-Cycle: Give or Trade Items Related to Breast Cancer
- 5.9K Clinical Trials, Research News, Podcasts, and Study Results
- 86 Coping with Holidays, Special Days and Anniversaries
- 828 Employment, Insurance, and Other Financial Issues
- 101 Family and Family Planning Matters
- Family Issues for Those Who Have Breast Cancer
- 26 Furry friends
- 1.8K Humor and Games
- 1.6K Mental Health: Because Cancer Doesn't Just Affect Your Breasts
- 706 Recipe Swap for Healthy Living
- 704 Recommend Your Resources
- 171 Sex & Relationship Matters
- 9 The Political Corner
- 874 Working on Your Fitness
- 4.5K Moving On & Finding Inspiration After Breast Cancer
- 394 Bonded by Breast Cancer
- 3.1K Life After Breast Cancer
- 806 Prayers and Spiritual Support
- 285 Who or What Inspires You?
- 28.7K Not Diagnosed But Concerned
- 1K Benign Breast Conditions
- 2.3K High Risk for Breast Cancer
- 18K Not Diagnosed But Worried
- 7.4K Waiting for Test Results
- 603 Site News and Announcements
- 560 Comments, Suggestions, Feature Requests
- 39 Mod Announcements, Breastcancer.org News, Blog Entries, Podcasts
- 4 Survey, Interview and Participant Requests: Need your Help!
- 61.9K Tests, Treatments & Side Effects
- 586 Alternative Medicine
- 255 Bone Health and Bone Loss
- 11.4K Breast Reconstruction
- 7.9K Chemotherapy - Before, During, and After
- 2.7K Complementary and Holistic Medicine and Treatment
- 775 Diagnosed and Waiting for Test Results
- 7.8K Hormonal Therapy - Before, During, and After
- 50 Immunotherapy - Before, During, and After
- 7.4K Just Diagnosed
- 1.4K Living Without Reconstruction After a Mastectomy
- 5.2K Lymphedema
- 3.6K Managing Side Effects of Breast Cancer and Its Treatment
- 591 Pain
- 3.9K Radiation Therapy - Before, During, and After
- 8.4K Surgery - Before, During, and After
- 109 Welcome to Breastcancer.org
- 98 Acknowledging and honoring our Community
- 11 Info & Resources for New Patients & Members From the Team