Tissue Remaining After Mastectomy
I am curious to know if women have discussed how much tissue would remain after mastectomy with their breast surgeons. I interviewed my 5th breast surgeon yesterday. He indicated that 7mm of breast tissue would remain attached to the skin for my Nipple Sparing Mastectomy with DIEP Reconstruction. None of the other surgeons I spoke to addressed this with me. I am curious to know if this is normal or what others have encountered. Thanks and Happy New Year.
Comments
-
Are they talking about the fatty/connective tissue that lies under the skin and gives the breast shape and structure, or actual breast (glandular) tissue which consists of the lobules and ducts? Because those aren't the same thing.
On this diagram, you can see the fatty tissue underlying the skin (the yellow fatty-looking substance) and then the ducts and lobules in the centre:

In a prophylactic mastectomy the idea is to remove as much of the glandular tissue as possible. Surgeons (unless they are or need to be particularly aggressive) will leave a layer of fatty/connective tissue in a skin sparing procedure as the fatty tissue "smooths" out the remaining skin over, say, an implant, and reduces risk of skin necrosis for example. In this diagram of a reconstruction with a TE/implant you can see a fat layer under the skin, followed by muscle before the TE, but the glandular tissue is (mostly) removed:
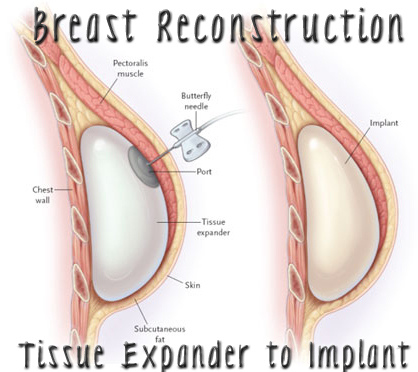
I know you are doing DIEP, but the implant images show this skin and subcutanous fat layer the best! With DIEP, your flap will be OVER the muscle and right under the skin/subcutaneous fat. Remember a big part of this is preserving blood flow to skin, and for you...connecting blood flow to the flap, so you do not usally want too thin of a skin flap.
If you are doing a prophylactic surgery, usually a bit more fatty tissue may be left as there is not a concern with excising a tumour or local spread into surrounding fatty tissues or skin. Indeed, some women who have an mx on one side as treatment, and a mx on the other side as as prophylactic, sometimes may notice a difference in the "thickness" of their skin over an implant compared to the other side.
So, it sounds like your surgeon is talking about leaving about 7mm (just over 1/4") of subcutaneous fat behind under the skin. I do think this is fairly common for prophylactic skin-sparing mastectomies, though some surgeons may prefer to leave even thinner skin flaps than others. It is good you are talking to your surgeon to know what to expect, though I think most do not talk to much about how much fat they leave underneath but this may depend on the patient too. My main concern was how much glandular tissue they may leave and we thorougly discussed this aspect.
Cosmetic results are important to me, as is obviously reducing risk of skin necrosis and such, but I know in talking with my breast surgeon and plastic surgeon they are very experienced and will remove as much glandular tissue as they can while leaving enough subcutanous fat to support the skin and so forth...but how much they do leave may depend a bit on what is in there when they get in there. I am not so concerned about whether it is 5 mm or 7 mm, as long as they trust they removed as much glandular tissue as they could and did not leave some behind just in order to leave more subcutaneous fat...and yet leave enough to keep good blood flow and so forth (I am having implants, not DIEP). My breast surgeon did say that it did depend a lot on what they saw when they got in there, but that he (working with plastic surgeon) do keep cosmetics in mind too and don't just go for as thin of a skin flap as possible!
Both of the breast surgeons I have seen explained to me that the small amount of glandular (breast) tissue that remains tends to be in the upper outer side of the breast near and into the armpit, where it is rather intermingled with the axillary nodes and difficult to remove it all because they are not removing nodes. If you look at this diagram, you will see the area I mean in the upper left:
Hmm, that picture seems to not be working now..so ETA new photo, but now nodes are in upper right area (the images upper left breast):

This does not mean glandular may not remain elsewhere. I am not planning on a nipple-sparing though so far. They did explain with a nipple sparing that I could expect more tissue to remain behind the nipple/areola as well. Some surgeons will core the nipple, others will not. A prophylactic mastectomy (or any mastectomy) does not remove ALL glandular tissue, so self-exams and other exams as discussed with your doctor remain important.
-
Thank you so much for your detailed response!! He was talking about the subcutaneous fat that lies beneath the dermis of the skin for a NS PBM w/ DIEP. The pictures are so helpful. I scoured the internet and found nothing on this topic.
Best,
Anne
-
Hi,
Thanks to DiveCat for the image explaining how much tissue should remain. All surgeons seem to have their own ideas,
about how much tissue should remain. What is the optimal removal? Is it better doing, if you have the chance and a strong will,
to remove the boobs, with no reconstruction? - if there is already LCIS or papilloma for example?As LCIS is not often seen on imaging
or even by the naked eye. If you do no reconstruction, you may still be able to do biopsies in the area, which would not be possible
if the "silikon stuff" implants were put there. Do implants make it difficult for mammograms, seeing ev new lesions?
How stupid of me, LCIS is seldom seen on imaging.
Take care
-
I think most surgeons would agree removing as much glandular tissue as possible is optimal, but how much is optimal depends on various other factors...like the woman's own body, whether she is keeping the nipple, how much glandular tissue they can remove without compromising skin, etc.
You can still get biopsies with implants. A friend of mine who had a PBMX with implant reconstruction due to being BRCA+ had a biopsy a few weeks ago (benign, fortunately!).
Implants also actually tend to push and the breast tissue forward and make it easier to monitor lumps and bumps...as they are under the chest muscle. Screening after implants depends on woman and her medical team. Mammograms in past were not generally done where there was implant reconstruction but some centres do now seem to provide mammograms anyway in these cases. I imagine it takes a bit of finesse though. MRIs, ultrasounds,mCBEs, and self-exams may still be recommended (some or all).
I do not think there is any "better" as it is up to each woman and depends on her, her own risk, her personal tolerance of risk, her personal and family history, and so on. I certainly do not think the immediate reaction to LCIS needs to be to get an MX. LCIS is usually a secondary finding, but not all (or even most) women need to remove their breasts for LCIS nor would it be "better" to do so. It is a risk factor for cancer, but is not itself cancer or a guarantee of future cancer and indeed it appears studies show the majority of women with LCIS do not develop cancer. It is up to each woman to decide in discussion with her doctors.
-
Man thats an awesome post!
-
Anne... This is an interesting question. When I went to a consultation with Dr Allen in NYC, he said he asks his BS to retain breast fat thus not needing to harvest as much fat. I asked my local BS if this was even possible to do AND get as much breast tissue as possible, and she said NO. So then when I consulted with Dr DellaCroce in NOLA and asked him about it, he said his BS strips the breast of all breast tissue. And also said he gets a lot of patients who had MX's elsewhere who have had too much tissue left behind and they have to re-do the MX. I believe (and maybe it was you who asked) that on the ASK THE DOCTOR forum, Dr D answers this question.
-
yup, Dr, D answered my question on ask the Dr. :-)
-
I am 7 weeks post bilateral mastectomy and seeing that a lot of tissue was left behind in one breast. Is there reason to fear that all the breast tissue was not removed? I see the surgeon again in two weeks and will ask her. She has left a lot of skin, perhaps believing that I want reconstruction, which I don't. I fear that I will have to go back for a revision. Has this happened to others?
-
Yes, the same thing in my situation. I can feel what I think is breast tissue below the incision on both sides, and he left so much skin that I actually have two little "mounds"------my skin does not lie flat. I feel like he did this thinking that I would want reconstruction later on. At a 4 week follow up appointment, he told me that he could correct the appearance after 6 months post surgery. Ugghhh!
-
Em hello cat friend and deeE
I just found out your post. I am in the same situation. My bilateral mastectomy done in December 2017. Immediate after surgery I found out that Dr left tissues on both sides and below of the breasts. Breast curve still there. Dr said its going to be ok after 3/4 months. It's been 5 months , no change at all. I am BRCA1 carrier, I am afraid if it's ok to leave that much tissue behind. My onclogist not happy with that.
Did you do anything? Is there any risk? Thanks .
Categories
- All Categories
- 679 Advocacy and Fund-Raising
- 289 Advocacy
- 68 I've Donated to Breastcancer.org in honor of....
- Test
- 322 Walks, Runs and Fundraising Events for Breastcancer.org
- 5.6K Community Connections
- 282 Middle Age 40-60(ish) Years Old With Breast Cancer
- 53 Australians and New Zealanders Affected by Breast Cancer
- 208 Black Women or Men With Breast Cancer
- 684 Canadians Affected by Breast Cancer
- 1.5K Caring for Someone with Breast cancer
- 455 Caring for Someone with Stage IV or Mets
- 260 High Risk of Recurrence or Second Breast Cancer
- 22 International, Non-English Speakers With Breast Cancer
- 16 Latinas/Hispanics With Breast Cancer
- 189 LGBTQA+ With Breast Cancer
- 152 May Their Memory Live On
- 85 Member Matchup & Virtual Support Meetups
- 375 Members by Location
- 291 Older Than 60 Years Old With Breast Cancer
- 177 Singles With Breast Cancer
- 869 Young With Breast Cancer
- 50.4K Connecting With Others Who Have a Similar Diagnosis
- 204 Breast Cancer with Another Diagnosis or Comorbidity
- 4K DCIS (Ductal Carcinoma In Situ)
- 79 DCIS plus HER2-positive Microinvasion
- 529 Genetic Testing
- 2.2K HER2+ (Positive) Breast Cancer
- 1.5K IBC (Inflammatory Breast Cancer)
- 3.4K IDC (Invasive Ductal Carcinoma)
- 1.5K ILC (Invasive Lobular Carcinoma)
- 999 Just Diagnosed With a Recurrence or Metastasis
- 652 LCIS (Lobular Carcinoma In Situ)
- 193 Less Common Types of Breast Cancer
- 252 Male Breast Cancer
- 86 Mixed Type Breast Cancer
- 3.1K Not Diagnosed With a Recurrence or Metastases but Concerned
- 189 Palliative Therapy/Hospice Care
- 488 Second or Third Breast Cancer
- 1.2K Stage I Breast Cancer
- 313 Stage II Breast Cancer
- 3.8K Stage III Breast Cancer
- 2.5K Triple-Negative Breast Cancer
- 13.1K Day-to-Day Matters
- 132 All things COVID-19 or coronavirus
- 87 BCO Free-Cycle: Give or Trade Items Related to Breast Cancer
- 5.9K Clinical Trials, Research News, Podcasts, and Study Results
- 86 Coping with Holidays, Special Days and Anniversaries
- 828 Employment, Insurance, and Other Financial Issues
- 101 Family and Family Planning Matters
- Family Issues for Those Who Have Breast Cancer
- 26 Furry friends
- 1.8K Humor and Games
- 1.6K Mental Health: Because Cancer Doesn't Just Affect Your Breasts
- 706 Recipe Swap for Healthy Living
- 704 Recommend Your Resources
- 171 Sex & Relationship Matters
- 9 The Political Corner
- 874 Working on Your Fitness
- 4.5K Moving On & Finding Inspiration After Breast Cancer
- 394 Bonded by Breast Cancer
- 3.1K Life After Breast Cancer
- 806 Prayers and Spiritual Support
- 285 Who or What Inspires You?
- 28.7K Not Diagnosed But Concerned
- 1K Benign Breast Conditions
- 2.3K High Risk for Breast Cancer
- 18K Not Diagnosed But Worried
- 7.4K Waiting for Test Results
- 603 Site News and Announcements
- 560 Comments, Suggestions, Feature Requests
- 39 Mod Announcements, Breastcancer.org News, Blog Entries, Podcasts
- 4 Survey, Interview and Participant Requests: Need your Help!
- 61.9K Tests, Treatments & Side Effects
- 586 Alternative Medicine
- 255 Bone Health and Bone Loss
- 11.4K Breast Reconstruction
- 7.9K Chemotherapy - Before, During, and After
- 2.7K Complementary and Holistic Medicine and Treatment
- 775 Diagnosed and Waiting for Test Results
- 7.8K Hormonal Therapy - Before, During, and After
- 50 Immunotherapy - Before, During, and After
- 7.4K Just Diagnosed
- 1.4K Living Without Reconstruction After a Mastectomy
- 5.2K Lymphedema
- 3.6K Managing Side Effects of Breast Cancer and Its Treatment
- 591 Pain
- 3.9K Radiation Therapy - Before, During, and After
- 8.4K Surgery - Before, During, and After
- 109 Welcome to Breastcancer.org
- 98 Acknowledging and honoring our Community
- 11 Info & Resources for New Patients & Members From the Team