High dose cholecalciferol (Vitamin D3)
Comments
-
My GP (regular doctor) has suggested that I take cholecalciferol (Vitamin D3) 1.25mg (50,000 IU) one tablet monthly. I am NED now and I am on no other medication, just completing my reconstruction post UMX. I am pre menopausal - not sure whether to take or not. I have seen that some people take it and I also believe it may prevent breast cancer! Any thoughts much appreciated.
-
Hi Hils,
If you're interested, you can read about what the main Breastcancer.org site says about Vitamin D and if there are any risks involved and what the research says.
Hope this helps!
--The Mods
-
Cheers Mods
-
Be careful with the 50,000 IU of "D3"... Many have reported on these threads that the doc prescribes D3 but the pharmacist fills it with D2 because according to their pharmacological book it is the same. It is not the same. Your body must convert the D2 to D3 and many are low on D3 because their bodies don't convert it very well.
I take D3 every day. Had to take 20,000 IU per day to get my level up. I apparently don't absorb it very well. Am really trying to get it from the natural sun to get all the benefits.
Anyway, my husbands doc prescribed him 50,000 IU D3 per week for a month. I checked with the pharmacist and sure enough he said he prescribed D2 because D3 doesn't come in 50,000 doses.
A few women on here have said their 50,000 IU prescription is in fact D3.
There was a study I read about where they gave elderly folks a really high dose .. I think 125,000 or 150,000 dose once a year. Worked great except it caused them to get dizzy and fall down which as you know isn't good for the elderly. So, they dropped that idea.
-
Hi Luna 5, thanks for all of your information, very interesting. Having read yours and some other information I have decided to walk away from these tablets. My GP(Physician) has not carried out any blood tests to see if I have low levels of D3 so I think to take it blind is not a sensible approach. Plus I do not see any benefits in taking medication just for the sake of it, when as with any medication there is side effects.
Thanks everyone for helping me think through this properly. Have a great week
-
Taken form Orac's blog today:
Supplements: Not mystical anticancer magic
Finally, Martinez et al take on the case of vitamin D and calcium. Anyone who's been reading CAM-friendly websites these days probably knows that vitamin D is currently viewed by many in the alternative medicine world as some sort of panacea that prevents all cancer. Heck, to listen to some CAM advocates tell it, vitamin D is supposedly so awesome that it prevents influenza more effectively than the influenza vaccine. Of course, as has been pointed out before, the picture is, as is usually the case, more complicated than that, and Martinez et al try to communicate that complexity, referencing the Institute of Medicine's recent recommendations for vitamin D and calcium intake published in 2011, in which the IOM concluded that there is insufficient evidence to conclude that there is a causal association between low vitamin D intake or low blood 25 hydroxy (OH) vitamin D [25(OH)D] levels and cancer. Martinez et al sum up this data thusly:
There have been many epidemiological investigations of blood 25 hydroxy (OH) vitamin D [25(OH)D] concentrations and cancer-related endpoints (45-49), and meta-analyses of these have shown statistically significant inverse associations between serum 25(OH)D and colorectal adenoma (46,49) and colorectal cancer (45), whereas the results for prostate cancer have largely been null (45,48). For breast cancer, the relationship with serum 25(OH)D levels varies by study design; case-control studies generally demonstrate inverse associations, and prospective studies have been null (45,47,50); because blood levels are collected after the onset of cancer in case-control studies, the potential for bias in these studies must be considered (47,50). Clearly, clinical trials are needed to elucidate any preventive effect of vitamin D (51,52). To date, three short-term RCTs of vitamin D and cancer endpoints (52-55) have been completed; one showed no direct effect of vitamin D supplementation on cancer mortality (53), the second showed no reduction in breast or colorectal cancer incidence by a vitamin D/calcium combination (54,55), and the third showed a reduction in total cancer incidence by a calcium/vitamin D combination vs placebo (56). As concluded in a recent meta-analysis, because of the potential confounding inherent in observational studies and the limited data from clinical trials, evidence is currently insufficient to draw conclusions about the efficacy of vitamin D supplementation for cancer prevention (57).
As far as cancer is concerned, there just isn't a whole lot of data from well-designed randomized clinical trials testing the effect of vitamin D supplementation on cancer risk to hang one's hat on. The same is true of calcium supplementation, only more so. Observational studies have, as Martinez et al almost drolly characterize it, "yielded diverse results." In any case some of the diverse results with respect to vitamin D suggest a correlation between high vitamin D concentrations and pancreatic cancer, while a recent meta-analysis suggests a reduction in risk. In the case of prostate cancer, however, a recently published study suggests a statistically significantly increased risk of prostate cancer (RR = 1.56 for men in the highest quintile) among men who have the highest levels of 25(OH)D, a finding that was more striking for aggressive disease, leading the authors of the study to advise caution in recommending vitamin D for cancer prevention. Puzzlingly, these results are in contrast to a lot of basic science research that supports a beneficial role for vitamin D compounds in prostate cell proliferation and differentiation, prostate cancer cell growth and invasion, and tumorigenesis. Clearly, as we say in the biz, more research will be needed to sort this out and figure out for which diseases, if any, vitamin D supplementation is helpful for prevention, what the potential risks might be in terms of increasing the risk of other diseases, and when it is appropriate to use. One thing's for sure: It's not going to be as simple as the alt-med quacks and supplement hucksters try to present it in their propaganda and advertising.
To say that the state of evidence in support of the use of various dietary supplements as cancer preventatives is unsettled is a gross understatement. Martinez et al discussed supplements that have been studied the most and, let's be frank, that involve the purest supplements, most of which contain only a single ingredient, and they found little evidence of efficacy in preventing cancer but some evidence of potential harm. That's not even counting the near innumerable supplements now being sold that are not pure substances but some form of extract from plant, fungi, yeast, or even animal origin. As I've said before time and time again, supplements that "work" (i.e., have some sort of biological effect) are drugs. They're impure, adulterated drugs with highly variable potency because of their highly variable content of active ingredient. Obviously, supplements that don't have such a biological effect are worthless (except for lining the pockets of supplement manufacturers). That's why supplement manufacturers very much want consumers to believe that their supplements have a whole range of beneficial biological effects, and the DSHEA allows them to imply that, as long as they don't do it too explicitly.
http://scienceblogs.com/insolence/2012/05/supplements_not_mystical_anticancer_magic.php#more
-
And there's this from Harriet Hall's (skepdoc) blog two years ago:
The IOM was asked by the US and Canadian governments to assess the current data on health outcomes associated with calcium and vitamin D. They formed a committee of experts who did an exhaustive review of over 1000 studies and listened to testimony from scientists and stakeholders. Their report, issued on 11/30/2010, concluded that the evidence supported a role for these nutrients in bone health but not in other health conditions, that the majority of the American and Canadian population is getting enough of both vitamin D and calcium, and that there is emerging evidence that an excess of these nutrients may be harmful. Based on that evidence, they established new Dietary Reference Intakes (DRIs) for vitamin D and calcium. They acknowledged exceptions and areas of uncertainty.
A couple of my correspondents have been screening their patients for vitamin D deficiency and they report that at least half fall in the "very low" category <20ng/mL. Doctors are giving large doses (often a weekly 50,000 IU pill for several weeks) to quickly get their patients back into the "normal" range. Then a 2000 IU or even a 5000 IU daily dose can be necessary to keep them at that level. Are they treating a true deficiency? Or are they uselessly trying to move people from one side of a normal bell curve to the other? When half of our patients fall into the "abnormal" category, it bothers me.
The IOM report explains
the measurements, or cut-points, of sufficiency and deficiency used by laboratories to report results have not been set based on rigorous scientific studies, and no central authority has determined which cut-points to use. A single individual might be deemed deficient or sufficient, depending on the laboratory where the blood is tested. The number of people with vitamin D deficiency in North America may be overestimated because many laboratories appear to be using cut-points that are much higher than the committee suggests is appropriate.
There can be too much of a good thing. Gary Null inadvertently sounded a note of caution when he managed to poison himself with one of his own products. The manufacturer of Null's Ultimate Power Meal supplement got the math wrong (by a factor of a thousand, no less!) and overloaded the supplement with 2,000,000 IU of vitamin D instead of 2000 IU. Null nearly died. The IOM recommends an upper limit of 4000 IU a day.Calcium supplements, long recommended to prevent osteoporosis, have been associated with heart attacks in postmenopausal women, but only in those who took it without the recommended addition of vitamin D. There are concerns that excess calcium might cause kidney stones and other adverse effects. The IOM found that most people get enough calcium from their diet, with the exception of girls ages 9-18, and that postmenopausal women who take supplements may be getting too much calcium. Once intakes exceed 2000 mg a day, the risk for harm increases.
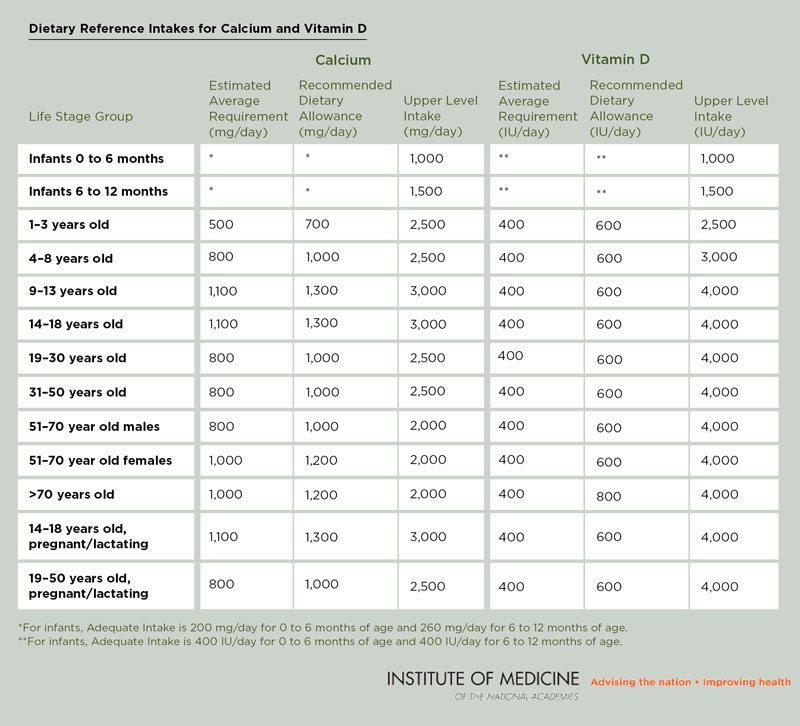
This table shows the new recommendations for calcium and vitamin D for different age groups.
As we continue to learn more about nutrition, the DRIs will continue to change. Science is a work in progress. The IOM has not given us a final answer, but it has offered reasonable science-based interim guidance. I'll take its advice over that of Walmart any day.
http://www.sciencebasedmedicine.org/index.php/new-recommendations-for-calcium-and-vitamin-d-intake/
Categories
- All Categories
- 679 Advocacy and Fund-Raising
- 289 Advocacy
- 68 I've Donated to Breastcancer.org in honor of....
- Test
- 322 Walks, Runs and Fundraising Events for Breastcancer.org
- 5.6K Community Connections
- 282 Middle Age 40-60(ish) Years Old With Breast Cancer
- 53 Australians and New Zealanders Affected by Breast Cancer
- 208 Black Women or Men With Breast Cancer
- 684 Canadians Affected by Breast Cancer
- 1.5K Caring for Someone with Breast cancer
- 455 Caring for Someone with Stage IV or Mets
- 260 High Risk of Recurrence or Second Breast Cancer
- 22 International, Non-English Speakers With Breast Cancer
- 16 Latinas/Hispanics With Breast Cancer
- 189 LGBTQA+ With Breast Cancer
- 152 May Their Memory Live On
- 85 Member Matchup & Virtual Support Meetups
- 375 Members by Location
- 291 Older Than 60 Years Old With Breast Cancer
- 177 Singles With Breast Cancer
- 869 Young With Breast Cancer
- 50.4K Connecting With Others Who Have a Similar Diagnosis
- 204 Breast Cancer with Another Diagnosis or Comorbidity
- 4K DCIS (Ductal Carcinoma In Situ)
- 79 DCIS plus HER2-positive Microinvasion
- 529 Genetic Testing
- 2.2K HER2+ (Positive) Breast Cancer
- 1.5K IBC (Inflammatory Breast Cancer)
- 3.4K IDC (Invasive Ductal Carcinoma)
- 1.5K ILC (Invasive Lobular Carcinoma)
- 999 Just Diagnosed With a Recurrence or Metastasis
- 652 LCIS (Lobular Carcinoma In Situ)
- 193 Less Common Types of Breast Cancer
- 252 Male Breast Cancer
- 86 Mixed Type Breast Cancer
- 3.1K Not Diagnosed With a Recurrence or Metastases but Concerned
- 189 Palliative Therapy/Hospice Care
- 488 Second or Third Breast Cancer
- 1.2K Stage I Breast Cancer
- 313 Stage II Breast Cancer
- 3.8K Stage III Breast Cancer
- 2.5K Triple-Negative Breast Cancer
- 13.1K Day-to-Day Matters
- 132 All things COVID-19 or coronavirus
- 87 BCO Free-Cycle: Give or Trade Items Related to Breast Cancer
- 5.9K Clinical Trials, Research News, Podcasts, and Study Results
- 86 Coping with Holidays, Special Days and Anniversaries
- 828 Employment, Insurance, and Other Financial Issues
- 101 Family and Family Planning Matters
- Family Issues for Those Who Have Breast Cancer
- 26 Furry friends
- 1.8K Humor and Games
- 1.6K Mental Health: Because Cancer Doesn't Just Affect Your Breasts
- 706 Recipe Swap for Healthy Living
- 704 Recommend Your Resources
- 171 Sex & Relationship Matters
- 9 The Political Corner
- 874 Working on Your Fitness
- 4.5K Moving On & Finding Inspiration After Breast Cancer
- 394 Bonded by Breast Cancer
- 3.1K Life After Breast Cancer
- 806 Prayers and Spiritual Support
- 285 Who or What Inspires You?
- 28.7K Not Diagnosed But Concerned
- 1K Benign Breast Conditions
- 2.3K High Risk for Breast Cancer
- 18K Not Diagnosed But Worried
- 7.4K Waiting for Test Results
- 603 Site News and Announcements
- 560 Comments, Suggestions, Feature Requests
- 39 Mod Announcements, Breastcancer.org News, Blog Entries, Podcasts
- 4 Survey, Interview and Participant Requests: Need your Help!
- 61.9K Tests, Treatments & Side Effects
- 586 Alternative Medicine
- 255 Bone Health and Bone Loss
- 11.4K Breast Reconstruction
- 7.9K Chemotherapy - Before, During, and After
- 2.7K Complementary and Holistic Medicine and Treatment
- 775 Diagnosed and Waiting for Test Results
- 7.8K Hormonal Therapy - Before, During, and After
- 50 Immunotherapy - Before, During, and After
- 7.4K Just Diagnosed
- 1.4K Living Without Reconstruction After a Mastectomy
- 5.2K Lymphedema
- 3.6K Managing Side Effects of Breast Cancer and Its Treatment
- 591 Pain
- 3.9K Radiation Therapy - Before, During, and After
- 8.4K Surgery - Before, During, and After
- 109 Welcome to Breastcancer.org
- 98 Acknowledging and honoring our Community
- 11 Info & Resources for New Patients & Members From the Team