Zometa for reducing chance of recurrence
Something to consider....Since women with Her2+ breast cancer may consider themselves at increased risk for recurrence - they may want to consider taking zometa 2x per year as was done in the ABCSG-12 study described below. Zometa reduced recurrence by about 36%. Many of us diagnosed Her2+ BC take it (or a participating in a trial with similar drugs)
This is a repost.
Multiple studies are now demonstrating significant reduction in recurrence rates with zoledronic acid (brand name Zometa).
In premenopausal women, in study ABCSG-12, zoledronic acid reduced recurrence by 36%.
In postmenopausal women, in the integrated anaysis of the Z-fast and Zo-fast trials, zoldronic acid reduced recurrence by 43%
In the neoadjuvant subset of the AZURE trial zoledronic acid reduced tumor volume by 33% and doubled the pathologic complete response rate
From an article in Medscape 1/5/2010
http://www.medscape.com/viewarticle/713259_4
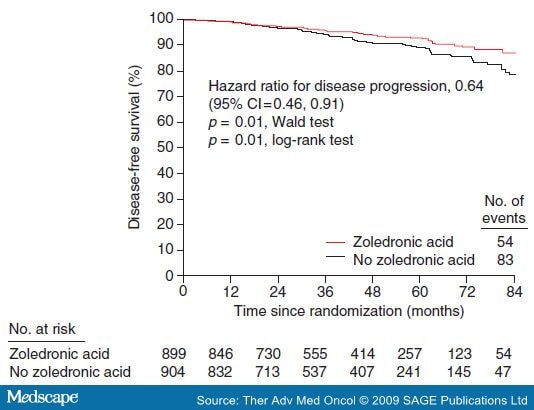
The ABCSG-12 trial compared tamoxifen with anastrozole and endocrine therapy alone with endocrine therapy plus ZOL (4 mg IV q6mo) in 1,803 premenopausal women with early stage endocrine-responsive breast cancer receiving ovarian suppression therapy with goserelin. The primary endpoint of ABCSG-12 was DFS for the comparison of anastrozole versus tamoxifen and ZOL versus no ZOL [Gnant et al. 2009]. At a median follow-up of 48 months, there was no significant difference in DFS for anastrozole versus tamoxifen (hazard ratio [HR]=1.10; p = 0.59) [Gnant et al. 2009]. In contrast, adding ZOL to adjuvant endocrine therapy significantly improved DFS by 36% compared with adjuvant endocrine therapy alone (54 versus 83 events; HR=0.64; log-rank p = 0.01; Figure 3) [Gnant et al. 2009]. Similarly, the secondary endpoint of recurrence-free survival was improved by 35% with ZOL treatment compared with endocrine therapy alone (54 versus 82 events; HR=0.65; log-rank p = 0.01) and produced a trend toward improved overall survival (16 versus 26 events; HR = 0.60; log-rank p = 0.10) [Gnant et al. 2009]. ZOL treatment reduced the incidence of bone metastases and decreased recurrence at all sites compared with adjuvant therapy alone. Moreover, ZOL was not significantly associated with serious adverse events, there were no confirmed cases of osteonecrosis of the jaw, and no renal tolerability issues were noted. Overall, adding ZOL to adjuvant endocrine therapy was generally well tolerated, reduced endocrine therapy-associated bone loss, and effectively improved clinical outcomes in pre-menopausal women with early stage breast cancer [Gnant et al. 2009; 2008; 2007].
Figure 3.
Bisphosphonates Improve Disease-free Survival in Premenopausal Women Receiving Adjuvant Endocrine Therapy with Goserelin Plus Tamoxifen or Anastrozole ± Zoledronic Acid. Adapted from Gnant et al. Copyright © 2009 Massachusetts Medical Society. All rights reserved [Gnant et al. 2009].
The effect of ZOL on disease recurrence and DFS in postmenopausal women with breast cancer was evaluated as a secondary endpoint in the three companion trials Z-FAST, ZO-FAST, and E-ZO-FAST [Frassoldati et al. 2009; Brufsky et al. 2008]. The 24-month integrated analysis of Z-FAST and ZO-FAST (total n = 1,667) demonstrated that upfront ZOL significantly improved DFS compared with delayed ZOL (HR= 0.573; p = 0.0183) [Frassoldati et al. 2009]. Similarly, the 36-month analysis of ZO-FAST (n = 1,064) found that patients in the upfront-ZOL group experienced reduced disease recurrence and improved DFS compared with patients in the delayed-ZOL group (HR = 0.588; p = 0.0314) [Eidtmann et al. 2008]. These exploratory data suggest that adding ZOL to AI therapy in postmenopausal women can improve disease outcomes beyond bone health.
In addition to the potential role in adjuvant therapy for breast cancer, the efficacy of bisphosphonates has been examined in combination with neoadjuvant chemotherapy. The neoadjuvant subset analysis (n = 205) from the ongoing AZURE trial (n = 3,360) examined the effect of neoadjuvant chemotherapy with or without ZOL on residual invasive tumor size and pathologic complete response in patients with stage II or III breast cancer. Patients who received neoadjuvant chemotherapy plus ZOL had a significant 33% reduction in residual invasive tumor size (p = 0.002) at the time of surgery and a nearly two-fold increase in pathologic complete response (p = 0.03) compared with standard therapy [Winter et al. 2008]. Furthermore, patients who received ZOL were less likely to require a mastectomy.
Categories
- All Categories
- 679 Advocacy and Fund-Raising
- 289 Advocacy
- 68 I've Donated to Breastcancer.org in honor of....
- Test
- 322 Walks, Runs and Fundraising Events for Breastcancer.org
- 5.6K Community Connections
- 282 Middle Age 40-60(ish) Years Old With Breast Cancer
- 53 Australians and New Zealanders Affected by Breast Cancer
- 208 Black Women or Men With Breast Cancer
- 684 Canadians Affected by Breast Cancer
- 1.5K Caring for Someone with Breast cancer
- 455 Caring for Someone with Stage IV or Mets
- 260 High Risk of Recurrence or Second Breast Cancer
- 22 International, Non-English Speakers With Breast Cancer
- 16 Latinas/Hispanics With Breast Cancer
- 189 LGBTQA+ With Breast Cancer
- 152 May Their Memory Live On
- 85 Member Matchup & Virtual Support Meetups
- 375 Members by Location
- 291 Older Than 60 Years Old With Breast Cancer
- 177 Singles With Breast Cancer
- 869 Young With Breast Cancer
- 50.4K Connecting With Others Who Have a Similar Diagnosis
- 204 Breast Cancer with Another Diagnosis or Comorbidity
- 4K DCIS (Ductal Carcinoma In Situ)
- 79 DCIS plus HER2-positive Microinvasion
- 529 Genetic Testing
- 2.2K HER2+ (Positive) Breast Cancer
- 1.5K IBC (Inflammatory Breast Cancer)
- 3.4K IDC (Invasive Ductal Carcinoma)
- 1.5K ILC (Invasive Lobular Carcinoma)
- 999 Just Diagnosed With a Recurrence or Metastasis
- 652 LCIS (Lobular Carcinoma In Situ)
- 193 Less Common Types of Breast Cancer
- 252 Male Breast Cancer
- 86 Mixed Type Breast Cancer
- 3.1K Not Diagnosed With a Recurrence or Metastases but Concerned
- 189 Palliative Therapy/Hospice Care
- 488 Second or Third Breast Cancer
- 1.2K Stage I Breast Cancer
- 313 Stage II Breast Cancer
- 3.8K Stage III Breast Cancer
- 2.5K Triple-Negative Breast Cancer
- 13.1K Day-to-Day Matters
- 132 All things COVID-19 or coronavirus
- 87 BCO Free-Cycle: Give or Trade Items Related to Breast Cancer
- 5.9K Clinical Trials, Research News, Podcasts, and Study Results
- 86 Coping with Holidays, Special Days and Anniversaries
- 828 Employment, Insurance, and Other Financial Issues
- 101 Family and Family Planning Matters
- Family Issues for Those Who Have Breast Cancer
- 26 Furry friends
- 1.8K Humor and Games
- 1.6K Mental Health: Because Cancer Doesn't Just Affect Your Breasts
- 706 Recipe Swap for Healthy Living
- 704 Recommend Your Resources
- 171 Sex & Relationship Matters
- 9 The Political Corner
- 874 Working on Your Fitness
- 4.5K Moving On & Finding Inspiration After Breast Cancer
- 394 Bonded by Breast Cancer
- 3.1K Life After Breast Cancer
- 806 Prayers and Spiritual Support
- 285 Who or What Inspires You?
- 28.7K Not Diagnosed But Concerned
- 1K Benign Breast Conditions
- 2.3K High Risk for Breast Cancer
- 18K Not Diagnosed But Worried
- 7.4K Waiting for Test Results
- 603 Site News and Announcements
- 560 Comments, Suggestions, Feature Requests
- 39 Mod Announcements, Breastcancer.org News, Blog Entries, Podcasts
- 4 Survey, Interview and Participant Requests: Need your Help!
- 61.9K Tests, Treatments & Side Effects
- 586 Alternative Medicine
- 255 Bone Health and Bone Loss
- 11.4K Breast Reconstruction
- 7.9K Chemotherapy - Before, During, and After
- 2.7K Complementary and Holistic Medicine and Treatment
- 775 Diagnosed and Waiting for Test Results
- 7.8K Hormonal Therapy - Before, During, and After
- 50 Immunotherapy - Before, During, and After
- 7.4K Just Diagnosed
- 1.4K Living Without Reconstruction After a Mastectomy
- 5.2K Lymphedema
- 3.6K Managing Side Effects of Breast Cancer and Its Treatment
- 591 Pain
- 3.9K Radiation Therapy - Before, During, and After
- 8.4K Surgery - Before, During, and After
- 109 Welcome to Breastcancer.org
- 98 Acknowledging and honoring our Community
- 11 Info & Resources for New Patients & Members From the Team