Pain and Other Things
Comments
-
Marijuana: Well isn't this just fun. Maybe the Government well get the hell out of the way.
https://community.breastcancer.org/forum/73/topics/840463?page=1#post_4617216
-
Sas,
I in no way meant to imply people don't get into level 10 pain. I had my L4/L5 disc rupture in my early 30's and couldn't walk. The pain was so bad that if I couldn't get relief I would have killed myself. That's my measure of level 10. I had to wait three days to get into surgery and they were the longest days of my life.
Waking from surgery is almost always a 8-9 for me for a couple of days. My normal is 4-6 and I've been treated for pain quite awhile now. NSAIDS damaged my GI tract and nearly killed me from peritonitis in my 40's, so I've been stuck with narcotics and non-medication choices. I think by your definition, staying at 4-6 is high, but I'm in constant pain. My back and hip joints are bad. Not to mention now healing from my Foobs. I'm having my right hip replaced 2/10/16. I'm quite freaked out by having another surgery, but I can hardly walk. The left was botched in 2010, and left me with Meralgia Parasthetica. It was revised 2013 and the stem hadn't integrated into the bone as it was too small and retroverted. I finally had the Lat. femoral nerve cut to stop signaling. Nothing else worked. The nerve is slowly coming back and pain with it.
And I am considering using the CBD part of marijuana. THC is risky for ER+ cancer. But it's legal here.
I'm close to my Pain Management Dr. And one of his beefs was people appearing to walk and sit comfortably , yet declaring they have level 10 pain. Those people are the ones who make it harder for we who have legitimate needs to get medications for our conditions.
I'm glad to share my experiences as part of your thread. Some things that work the best for pain are non-drug. Distraction tops the list. I also live at the local warm water pool. Sometimes I can't do much but float around, but I'm moving, and meeting others with their own issues which helps keep me off my pity pot.
I think you offer some great tools, and many cancer survivors end up with chronic pain. Dialoging about what things we use to help our pain is a wonderful idea
-
Leslie, your's is an important post for many reasons. Pain isn't just one thing/area/type in a chronic situation. Those of us with chronic pain would love to have 'just one area'. My joke when they ask me my pain level is 'which body part'. They laugh, I laugh. They want a number because it's required. They have one box. I'm serious, but know it's one box. They don't get that that's real re: which body part. Cynically, I know they're isn't much caring. They want to finish the interview and move on.
Let's get to your post. You have much to teach us. Your words. " I had my L4/L5 disc rupture in my early 30's and couldn't walk. The pain was so bad that if I couldn't get relief I would have killed myself. That's my measure of level 10. I had to wait three days to get into surgery and they were the longest days of my life.". This is over for you and I'm sorry that you had to experience this. You are an example of what I refer to as aggressive pain management in the hospital setting.
You should have been on several modalities to control your pain
1. Patient Controlled Analgesia PCA. It can be set at a maintenance dose with order for boluses at intervals if pain not controlled. That takes team work between the nurse and patient to make control happen.
2. Benzodiazipine muscle relaxer Valium. Has to be used carefully with a PCA because respiratory depression is a potential. General order is '5-10 mg every 6 hrs prn' This is a weakness generally on the nurses part. It's written as a prn( as necessary). The prn part is that they are to use 'judgement/critical analysis' to determine when to give. Not sure if in 2016 nurses have come to understand the beauty of Valium in skeletal muscle spasm. They can talk of it's antianxiety characteristics, but our generally 'brain void' of it's skeletal muscle action.
What happens when a bone causes pain, is the muscles around it go into protective mode. Spasm. This may have been protective in Neolithic times, now it's counterproductive. Spasming causes pain in and of itself. Causes a system response of increasing stress chemicals. Increases the inflammatory response. The whole body suffers.
Breaking the spasms associated with orthopedic problems helps with reducing pain. Judicious use of valium is important. Sadly, to many practitoners, don't understand this. This is something that should be carefully addressed with the doc preop and ask that direct instructions be given to the nurses.
I believe you went to the block thread. Ask your doc to determine what kind of localized blocks can be used. They're many. Injection of Marcaine directly into the incisional area. Localized infusing balls that deliver a 'caine' that directly affect the tissue. Generally used for 24-48(72) hours. They're may be more blocks that I don't know of.
The key is ask for a discussion. The beauty of these localized modalities allow you less use of systemic drugs. Safer approach.
Do you have a different orthopedic doc? Your words " The left was botched in 2010, and left me with Meralgia Parasthetica. It was revised 2013 and the stem hadn't integrated into the bone as it was too small and retroverted" I've been in the OR I've watched how they measure for the prosthesis. Too small, perhaps shouldn't have happened? Not familiar with the word retroverted in this context, but seems the sizing and placement wasn't done well. Hope a new doc is involved.
My description of a 4-6 in chronic pain is a middle ground. Us chronics learn to live there. For someone new to pain, they might describe it as greater. i.e. ten. Not to diminish them, but rookie painers (just made that up) have no reference and it is awful to them. If they get back to zero because every thing went right, they will always perceived it a 10. If they don't get back to zero, they will eventually slide into the 4-6 as the mind learns how to deal with it and become a chronic
For completeness, they're those that 10 is an issue as in Reflexive Sympathetic Dystrophy-RSD, now know as Chronic Regional Pain Syndrome-CRPS. Regretfully, these folks are in the 10 range. This an unusual pain syndrome. Hopefully discussed later.
With your pain doc that has a problem with people appearing to walk and sit comfortably and call themselves a ten. Ask him to review what is written here regarding the pain scale. Perhaps teaching them the basics of the scale will help.
But he is very right. They're are physical signs of pain that went put together with the pain scale can quide how pain is managed. I often just observe people walking across a parking lot and I can pick out hip, knee, back problems just by how they walk. There deliberateness of how they walk gives me a clue how much pain they are in.
-
Leslie, your words again " Some things that work the best for pain are non-drug. Distraction tops the list. I also live at the local warm water pool. Sometimes I can't do much but float around, but I'm moving, and meeting others with their own issues which helps keep me off my pity pot."
They following is for everyone. Pick and choose what works for you.
Warm water, warm water, warm , warm...........Warm moist heat if a pool isn't available.
Heat is wonderful for stressed muscles. Earlier I stated relaxing muscles is important. The are designed to stabilize the body. Believe it or not muscle tensing to the point of spasming is a protective mechanism. Spasm is a the far end of the extreme and it is painful depending on how strong the spasm is. Plus, prolonged muscle tenseness is very fatiguing to the muscle. Muscles just plum don't work right when it is so over used. You will see more spasming when the muscle reaches the end stage of fatigue.
Avoiding spasm is important, by recognizing that muscle fatigue is your real enemy.
Develop a plan to avoid muscle fatigue. Sounds easy, but may take work.
1. avoid long or even moderator time periods of doing one thing.
2. if your body is telling you it's unhappy doing something change your activity
3. don't allow yourself to get cold.
-
Leslie Your words again " Distraction tops the list." Please, describe in detail the situations that cause you to use distractions and what they are besides warm water. Thanks, don't think your stories long. You never know when a description triggers in another a recognition that it applies to them.
 Thanks.
Thanks. -
sas-schatzi, Love this thread. Such a wealth of information
-
Oh well, Thank you LadyB appreciate your appreciation !
-
This is a very informative thread and after reading all the inputs I think it might appropriately be called the Science of pain: origin and treatment. A separate thread might evolve called the Human experience of pain: Personal and up close where the voice of the human experiencing the situation is central and not distanced by layers of empirical data (that have their place) but do not stand in stead of the human before us experiencing the event. I recall an early encounter with a person so nauseated she could not eat but when describing this subjective symptom of nausea to my colleague the response was 'let me know when she throws up, then I have some measurable data to interpret. It is outrageous if we forget the human being before us who may or may not fall into a statistical norm.
-
Magic Hi welcome here, Saw your post and been mulling it over. You make allot of great points. Eventually it will happen here. I can say that with surety because I've done it before on several threads. My approach is to lay the groundwork. Then once it's done, move on to conversation. The groundwork here is to describe a historical perspective on pain management. Then the tools to get someone going on how to document their pain and communicate the info to their care team.
The historical look is important b/c even now in 2016 the average doc and nurse does not help manage pain as good as it can be done. Unless folks/patients understand this, they won't know this weakness is pervasive. Then we can learn how to train our docs & nurses to manage our pain well. They're has been great advancements since the 1980's, but we can do better.
Take a look at the Constipation thread. 30 some pages talking poop. I started with the technical and then it took off from there. It incorporates Evidenced Based material, Complimentary/ Alternative, and punning.
I'm starting off slow, b/c I'm slowing down these days. Would welcome you to stay and post material too. On the constipation thread they're several that mentor on that thread. Same with the Toradol thread, and Pinktober. In each place members have an interest.
https://community.breastcancer.org/forum/6/topics/781867?page=1 constipation thread
https://community.breastcancer.org/forum/73/topics/833612?page=1 Toradol thread.
-
Thanks for both of your threads Sass
Rosieo
-
Ah reminded me they're should be a poop column on the pain chart
Hi Rosieo, nice to see you
 Anything you need help with?
Anything you need help with? -
I promised Mags I'd work on Fibromyalgia. This is from Medscape. Copying it mostly in it's entirety for many reasons. Links break and it's easier to reference in the future. This was published Oct of 2015 and is the most current info re :Fibro. For those with Fibro dx already, much of this is known material. For those that haven't had a workup, this will provide a guide as to what they should expect their practitioner to do in diagnostic workup. For example, in the section that discusses other diseases that should be ruled out. This thorough approach may not be done. By reviewing all this material you are better prepared to assure something isn't missed.
I have left a few sections out i.e. psychological ,psychometrics, diet. Please, refer to the full article.
This first post is an outline of the whole topic as it appears on Medscape. The posts after this expands on sections from the outline.
http://emedicine.medscape.com/article/329838-overview
Fibromyalgia-General Overview
- Author: Chad S Boomershine, MD, PhD; Chief Editor: Herbert S Diamond, MD more...
Updated: Oct 23, 2015
What would you like to print?Practice Essentials
Fibromyalgia is a disorder of chronic, widespread pain and tenderness (see the image below). It typically presents in young or middle-aged women but can affect patients of either sex and at any age.
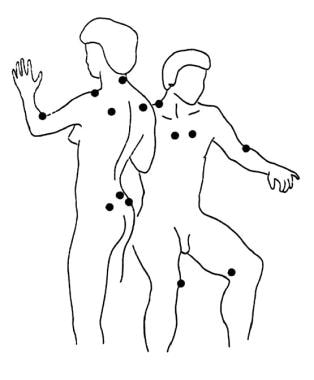 Tender points in fibromyalgia.
Tender points in fibromyalgia. See Fibromyalgia: Slideshow, a Critical Images slideshow, for more information on strategies for accurately diagnosing and treating fibromyalgia.
Signs and symptoms
Fibromyalgia is a syndrome that consists of the following signs and symptoms[1] :
- Persistent (≥ 3 mo) widespread pain (pain/tenderness on both sides of the body, above and below the waist, and includes the axial spine [usually the paraspinus, scapular, and trapezius muscles])
- Stiffness
- Fatigue; disrupted and unrefreshing sleep
- Cognitive difficulties
- Multiple other unexplained symptoms, anxiety and/or depression, and functional impairment of activities of daily living (ADLs)
See Clinical Presentation for more detail.
Diagnosis
"" frameborder="0" marginwidth="0" marginheight="0" scrolling="no" style="border: 0px currentColor; border-image: none; vertical-align: bottom;">Fibromyalgia is a diagnosis of exclusion and patients must be thoroughly evaluated for the presence of other disorders that could be the cause of symptoms before a diagnosis of fibromyalgia is made. The clinical assessment may reveal objective evidence for a discrete or comorbid illness, such as the following:
- Hypothyroidism
- Rheumatoid arthritis
- Systemic lupus erythematosus
- Polymyalgia rheumatic
- Other inflammatory or autoimmune disorders
- Serious cardiac conditions in those with chest pain, dyspnea, and palpitations
Laboratory testing
Although patients with fibromyalgia do not have characteristic or consistent abnormalities on laboratory testing, routine laboratory and imaging studies can help to rule out diseases with similar manifestations and to assist in diagnosis of certain inflammatory diseases that frequently coexist with fibromyalgia. Such tests include the following:
- Complete blood count with differential
- Metabolic panel
- Urinalysis
- Thyroid-stimulating hormone level
- 25-hydroxy vitamin D level
- Vitamin B12 level
- Iron studies, including iron level, total iron binding capacity, percent saturation, and serum ferritin level
- Magnesium level
- Erythrocyte sedimentation rate
- Antipolymer antibody assay: May provide conclusive evidence for a subgroup of people with fibromyalgia; about 50% of fibromyalgia patients have antipolymer antibodies
Patient self-report forms, clinical psychometric testing
Self-report forms, for assessing patients' pain, fatigue, and overall status, include the following:
- Modified Health Assessment Questionnaire
- Fibromyalgia Impact Questionnaire
- Checklist of current symptoms
- Scales for helplessness and cognitive performance
- The Physician Health Questionnaire - 9 for depression
- The Generalized Anxiety Disorder - 7 questionnaire for anxiety
- The Mood Disorder Questionnaire to screen for bipolar disease
Psychometric testing provides a more comprehensive assessment and includes the following:
- Minnesota Multiphasic Personality Inventory
- Social Support Questionnaire
- Sickness Impact Profile
- Multidimensional Pain Inventory
See Workup for more detail.
Management
There is no cure for fibromyalgia, but education, lifestyle changes, and proper medications can help the individual to regain control and achieve significant improvement.
Models of pain behavior that interrelate biologic, cognitive, emotional, and behavioral variables form the basis for cognitive-behavioral and operant-behavioral approaches to adult pain management. Fibromyalgia in children responds to a combination of psychotherapy, exercise, relaxation techniques, and education. Pharmacotherapy is generally not indicated in children.
Nonpharmacotherapy
- Diet (eg, promote good nutrition, vitamin supplementation, bone health, weight loss)
- Stress management
- Aerobic exercise (eg, low-impact aerobics, walking, water aerobics, stationary bicycle)
- Sleep therapy (eg, education/instruction on sleep hygiene)
- Psychologic/behavioral therapy (eg, cognitive-behavioral, operant-behavioral)
Pharmacotherapy
Always combine pharmacologic and nonpharmacologic therapy in the treatment of fibromyalgia. Aggressively treat comorbid depression.
Medications used in the management of fibromyalgia include the following:
- Analgesics (eg, tramadol)
- Antianxiety agents (eg, alprazolam, clonazepam, zolpidem, zaleplon, Trazodone, buspirone, temazepam, sodium oxybate)
- Skeletal muscle relaxants (eg, cyclobenzaprine)
- Antidepressants (eg, amitriptyline, duloxetine, milnacipran, venlafaxine, desvenlafaxine)
- Anticonvulsants (eg, pregabalin, gabapentin, tiagabine)
- Alpha 2 agonists (eg, clonidine)
Other agents used in fibromyalgia may include the following:
- Vitamins and minerals
- Malic acid and magnesium combination
- Antioxidants
- Amino acids
- Herbs and supplements
If nonpharmacotherapy fails to improve sleep problems, the following medications may help:
- Antidepressants (eg, trazodone, SSRIs, SNRIs, tricyclic antidepressants)
- Anticonvulsants (eg, clonazepam, gabapentin, tiagabine)
- Nonbenzodiazepine hypnotics (eg, zolpidem, zaleplon, eszopiclone)
- Muscle relaxants (eg, cyclobenzaprine, tizanidine)
- Dopamine agonists (eg, pramipexole)
See Treatment and Medication for more detail.
-
Workup Approach Considerations
The physician should inform the patient that no cure exists for fibromyalgia but that education, lifestyle changes including regular physical activity, and proper medications can help the individual to regain control and achieve significant improvement.[95] When patients with fibromyalgia fully understand the nature of the disease, they are more likely to comply with treatment and to take an active role in managing the disease.
At the initial visit, give patients educational materials about fibromyalgia, including a list of resources, such as Web sites, books, videotapes, newsletters, and brochures, related to the disease. Some authors recommend encouraging patients to attend their local fibromyalgia support group. Provide education and support to the patient's significant family members.
"" frameborder="0" marginwidth="0" marginheight="0" scrolling="no" style="border: 0px currentColor; border-image: none; vertical-align: bottom;">Therapeutic recommendations for fibromyalgia can now be based almost entirely on evidence from well-designed randomized controlled trials. Models of pain behavior that interrelate biologic, cognitive, emotional, and behavioral variables form the basis for cognitive-behavioral and operant-behavioral approaches to pain management. Wood published a useful summary of therapeutic approaches to central sensitivity syndrome (CSS) comorbidities in fibromyalgia.[96]
The first crucial element in the treatment of pain, fatigue, and other diverse symptoms in patients with fibromyalgia is for the clinician to validate the patient's illness through empathetic listening and acknowledgment that the patient is indeed experiencing pain.[26, 32, 97, 98, 99, 100, 101, 102, 103] Comments such as "it's all in your mind" or "I cannot find anything wrong with you" only add to the patient's frustration.
Avoid excessive use of physical therapy modalities after minor trauma, excessive activity limitation, and overly liberal work release. Be aware of confounders to recovery, such as pending litigation or compensation claims.
The overall approach for chronic pain in fibromyalgia involves a multifaceted treatment plan that incorporates various adjuvant medicines, aerobic and resistance exercise, and psychological and behavioral approaches to reduce distress and promote self-efficacy and self-management (eg, relaxation training, activity pacing, visual imagery, distraction).
If significant nociceptive pain coexists with the diffuse chronic pain of fibromyalgia, manage it pharmacologically with non-narcotic medications such as antidepressants, anticonvulsants, or muscle relaxers. For associated regional chronic pain syndromes (eg, temporomandibular disorder), referral to an experienced specialist who advocates nonsurgical approaches is recommended.
In a systematic review by Häuser of 1119 patients in 9 randomized controlled trials, multicomponent treatment (at least 1 form of educational or other psychological therapy plus at least 1 form of exercise therapy) yielded short-term benefits for the symptoms of pain, fatigue, depression, and quality of life. They found no evidence that these symptomatic benefits were durable in the long term, but strong evidence suggested that multicomponent therapy conferred a long-term benefit to maintenance of physical fitness.[104]
Poor sleep is virtually universal in fibromyalgia and contributes importantly to pain, depression, and fatigue. Accurate diagnosis and pharmacologic and nonpharmacologic management are essential.[105, 106, 107]
Trigger point injections, acupuncture, chiropractic manipulation, and myofascial release are usually well received by patients and can be beneficial, but results are not long lasting. In addition, patients may not be able to afford long-term therapy since these are sometimes not covered my insurance.
A possible etiologic link between Chiari malformation and fibromyalgia has been suggested. However, no generally accepted evidence indicates that skull surgery for correction of Chiari malformation is of benefit in patients with fibromyalgia and
Approach Considerations continuedPatients with fibromyalgia do not have characteristic or consistent abnormalities on laboratory testing. However, routine laboratory and imaging studies are important to help rule out diseases with similar manifestations and to assist in diagnosis of certain inflammatory diseases that frequently coexist with fibromyalgia. In addition to complete blood cell (CBC) count and differential count, basic metabolic panel, and urinalysis, the following limited evaluation is reasonable.
- Thyroid-stimulating hormone: Hypothyroidism shares many clinical features with fibromyalgia, especially diffuse muscle pain and fatigue
- 25-Hydroxy vitamin D level: Low levels can cause muscle pain and tenderness
- Vitamin B-12 level: Very low levels can cause pain and fatigue
- Iron studies including iron, total iron binding capacity, percent saturation, and serum ferritin: Low levels can cause fatigue and can lead to poor sleep and depressive symptoms; for patients with restless legs syndrome, percent saturation should be maintained above 20% and serum ferritin should be kept above 50 ng/mL
- Magnesium: Low levels can lead to muscle spasms, which are common in fibromyalgia patients; magnesium supplementation can also improve symptoms in some fibromyalgia patients; recommended magnesium levels in fibromyalgia patients are at least 2 mEq/L
The erythrocyte sedimentation rate (ESR) is often recommended as a routine laboratory test in fibromyalgia patients to rule out the presence of inflammatory disorders that may mimic symptoms. While the ESR is usually normal in patients with fibromyalgia, it is a nonspecific measure of inflammation and mild elevations may not be meaningful. The upper limit of normal for the ESR in women is half their age (eg, a level of 40 in an 80-year-old women is normal),and in men is half their age minus 10. The ESR can also be mildly elevated in obese patients. However, a high ESR may be indicative of an inflammatory disorder or occult malignancy that should be thoroughly evaluated.
"" frameborder="0" marginwidth="0" marginheight="0" scrolling="no" style="border: 0px currentColor; border-image: none; vertical-align: bottom;">Routine antinuclear antibody (ANA) or rheumatoid factor (RF) testing in not recommended unless patients have signs or symptoms concerning for systemic lupus erythematosus (SLE) or rheumatoid arthritis (RA). A low-titer positive ANA or RF level is common in the general population, so these findings may be of no clinical significance in a fibromyalgia patient.
Formal sleep studies may be useful in patients whose sleep does not improve with the usual conservative measures (eg, elimination of caffeine, prescription of hypnotics or nighttime tricyclics). These studies can be performed as part of a formal assessment by a neurologist or pulmonologist experienced in sleep disorders.
Serum transferrin saturation and serum ferritin screening can be useful for detecting the unusual cases of hemochromatosis in which patients present with diffuse arthralgias and myalgias. Consider screening with a serum transferrin saturation and a serum ferritin concentration in patients aged 40-60 years, especially those with small-joint arthropathy in the hands and/or calcium pyrophosphate dihydrate deposition disease (CPPD).
The antipolymer antibody assay is a blood test. Antipolymer antibodies are present in approximately 50% of patients with fibromyalgia. This biologic marker may provide conclusive evidence for a subgroup of people with fibromyalgia.
There are no histologic abnormalities seen in fibromyalgia syndrome. Earlier belief that fibromyalgia was associated with inflammation in muscle fascia has been disproven.
Carefully assess all possible causal or perpetuating factors. Investigate psychological and sociocultural factors and identify any specific regional sources of ongoing nociceptive pain (eg, degenerative spondylosis, bursitis).
-
Fibromyalgia Differential Diagnoses
- Author: Chad S Boomershine, MD, PhD; Chief Editor: Herbert S Diamond, MD more...
Updated: Oct 23, 2015
What would you like to print? Multimedia LibraryDiagnostic Considerations
Although no basis for many of the multiple symptoms of patients with fibromyalgia will be found upon physical examination or laboratory testing, the physician must remain alert for organic illness (eg, colon carcinoma in a patient with irritable bowel syndrome).
The clinical assessment may reveal objective evidence for a discrete illness, such as hypothyroidism, rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), polymyalgia rheumatica, or another inflammatory or autoimmune disorder. Such findings do not exclude comorbid fibromyalgia. Indeed, approximately 25% of patients with RA and approximately 50% of patients with SLE also have fibromyalgia, and the provision of optimum care in such cases impels recognition and treatment of both illnesses.
"" frameborder="0" marginwidth="0" marginheight="0" scrolling="no" style="border: 0px currentColor; border-image: none; vertical-align: bottom;">It is important to recognize that treatment of an autoimmune disorder in a patient with comorbid fibromyalgia usually does not improve fibromyalgia symptoms. Recognition and treatment of fibromyalgia in these patients is vitally important to avoid overtreatment with immunosuppressives that can result when providers falsely assume symptoms are caused by the autoimmune condition.
Other problems to consider in the differential diagnosis of fibromyalgia include the following:
- Atypical chest pain
- Chronic fatigue syndrome
- Multiple chemical sensitivity
- Sick building syndrome
- Vulvodynia
- Vulvar vestibulitis
Because complaints of chest pain, shortness of breath, and palpitations are common, serious cardiac problems should be considered and may require extensive evaluation. Many symptoms in patients with fibromyalgia can be related to mitral valve prolapse syndrome.
Differential Diagnoses
- Addison Disease
- Hepatitis C
- Hyperparathyroidism
- Hypochondriasis
- Hypothyroid Myopathy
- Malingering
- Personality Disorders
- Physical Medicine and Rehabilitation for Complex Regional Pain Syndromes
- Polymyalgia Rheumatica
- Posttraumatic Stress Disorder
-
Medication Summary
Medication summary
Always combine pharmacologic approaches with nonpharmacologic therapy in the treatment of fibromyalgia (FM), especially stress management, aerobic exercise, and, in some cases, psychotherapy. Aggressively treat comorbid depression.
"" frameborder="0" marginwidth="0" marginheight="0" scrolling="no" style="border: 0px currentColor; border-image: none; vertical-align: bottom;">Tricyclic antidepressants (TCAs) are of proven benefit. Certain anticonvulsants and antidepressants clearly decrease pain sensitivity. Corticosteroids and nonsteroidal anti-inflammatory medications are useful only as management for coexisting inflammatory processes. Pharmacologic and nonpharmacologic treatment of poor sleep is crucial for improving the patient's overall sense of well-being.
Anecdotally, dextromethorphan, an N -methyl-D-aspartate (NMDA) receptor antagonist available as an over-the-counter (OTC) antitussive, is beneficial as adjunctive therapy in patients with fibromyalgia. Topical capsaicin, obtained from red chili peppers, is essentially free of toxicity, other than mild burning at the site of application, and is useful as adjunctive therapy in combination with gentle massage.
Beta-blockers and/or increased fluid and sodium/potassium intake may benefit a subset of patients with fibromyalgia who have orthostatic hypotension, palpitation, and vasomotor instability. Growth hormone and cytokine therapies are still experimental.[119]
Patients with fibromyalgia have difficulty tolerating regular doses of most medications and supplements. They are sensitive to medications, and adverse effects are common. To avoid these problems, use the lowest dose available or perhaps one half to one quarter of the lowest recommended dose.
The US Food and Drug Administration (FDA) has approved three drugs for use in fibromyalgia: pregabalin (Lyrica), duloxetine (Cymbalta), and milnacipran (Savella). Pregabalin is used to reduce pain and improve sleep. The antidepressants duloxetine and milnacipran, which are used to relieve pain, fatigue, and sleep problems, are generally used at lower doses than for treatment of depression.
Several medications should be avoided or used carefully. Opioids, hypnotics, anxiolytics, and certain skeletal-muscle relaxants must be used with caution because of the potential for abuse.
A trial of tramadol may be considered for second-line therapy in patients with moderate to severe pain that is unresponsive to other treatments.[95, 120] In a 12-month observational study of opioid use in 1700 adult patients with fibromyalgia, tramadol proved superior to other opioids for improving pain-related interference with daily living, functioning, depression, and insomnia.[121]
Avoid complications and confusion by providing written instructions and drug information. These instructions need to be easy to understand. Patients should be instructed to consult their physician before starting any over-the-counter (OTC) medications or supplements, to avoid potentially harmful drug interactions.
Integrative medicine
Integrative medicine (complementary and altenative medicine [CAM]) is popular in patients with fibromyalgia, in part due to medical skepticism (ie, doubt in the ability of conventional medical care to appreciably alter health status).[122] Many physicians are ignorant of, if not overtly hostile toward, integrative medicine, and patients are often reluctant to inform their physician about their use of it. This can be dangerous because of unsuspected drug-to-drug interactions.
A practical approach is to inquire about integrative medicine usage, to refrain from expression of negative opinions if a particular integrative treatment is relatively inexpensive and appears to be safe, and to encourage whatever works in the context of the power of the placebo effect and promotion of self-efficacy for pain control.
Analgesics
Nonsteroidal anti-inflammatory drugs (NSAIDs) and acetaminophen are of limited efficacy in reducing pain due to fibromyalgia but are important adjuncts for nociceptive pain generators, such as osteoarthritis and degenerative spondylosis.[123] Topical anesthesia with lidocaine (5% Lidoderm patch) can also be helpful in this regard. Tramadol, a weak opioid agonist with additional effects on serotonin and norepinephrine receptors, improves pain associated with fibromyalgia.
Opioid analgesics with more potency (eg, hydrocodone, oxycodone, fentanyl, morphine), although frequently prescribed in patients with fibromyalgia, appear to be of limited efficacy in most patients with this disorder and are generally not recommended. However, in addition to utility in the treatment of severe nociceptive pain (eg, radicular pain, advanced osteoarthritis of the knee), opioid analgesics may reduce pain, improve quality of life, and occasionally restore function in a patient with fibromyalgia who has severe allodynia and who has not responded to other approaches.
More often, rheumatologists discover that patients with fibromyalgia are already taking very high doses of opioids prescribed by their family physician. The task is then to gradually withdraw opioids, if possible, or perhaps switch therapy to reasonable doses of methadone (eg, 5-10 mg tid). Tapering takes 2-3 weeks; clonidine, 0.2-0.4 mg/day, is helpful for controlling withdrawal symptoms. Remember that opioid-induced hyperalgesia can be a paradoxical complication of high-dose opioid therapy.
Monitoring of patients receiving opioid medications requires frequent reevaluation for efficacy, improvement in daily functioning, and adverse effects during initiation, titration, and maintenance therapy, especially in older patients. The patient should sign a "narcotics contract" that specifies the following:
- One prescribing physician
- One dispensing pharmacy
- Acceptance of no early prescription of opioids if the medication runs out early or is lost or stolen
- Agreement for random urine testing
Other medications
The selective estrogen receptor modulator raloxifene (Evista), 60 mg every other day, is effective in improving pain, improving fatigue, reducing tender-point count, and improving daily functioning in postmenopausal women with fibromyalgia.[124] Modafinil (Provigil), approved for narcolepsy and shift-work sleep disorder, 100-200 mg in the morning, improves fatigue and cognitive disturbances.[125, 126]
Preliminary data suggest that the synthetic cannabinoid nabilone (Cesamet) in doses escalating from 0.5 mg daily to 1 mg twice daily improves pain and anxiety in fibromyalgia.[127] Beta-adrenergic antagonists such as pindolol or propranolol (Inderal), given in low doses at bedtime, can also improve pain and agitation.[117]
Other medications used in fibromyalgia may include the following:
- Vitamins and minerals
- Malic acid and magnesium combination
- Antioxidants
- Amino acids
- Herbs and supplements
-
Fibro is not any easy disease and many diseases overlap or can be mistaken if evaluation and diagnosis systematically carried out.
http://www.fmcpaware.org/complete-listing-allergy-vulvodynia.html
Overlapping Conditions Directory
- The following is a list of conditions commonly associated with Fibromyalgia:
-
Wow, Sassy! You are a star!

Thank you for doing all the work on fibro. Since I have my first appointment at the pain center on Monday all this information is very timely. I'll try to read all the info by then. Wow, and double thank-you.

-
I suffer from fibromyalgia and pelvic pain. Due to vag atrophy I've had many UTIs. My PCP says that the atrophy is responsible for the pelvic pain and UTIs but she can't prescribe Vagifem due to my ER+ status. Instead she referred me to a urologist, a gyn and a pain center. I told her that my pain is often a 7 out of 10 and she recommended Tylenol. I've been at this level of pain for months with no relief. She will not prescribe opioids.
I go to the pain center in a couple of days after a month wait. The paperwork for the center includes an Opioid Treatment Agreement. I will have to sign a contract with them that says I agree to random drug screening tests and periodic random pill counts. I will not sell the medication or ask for early refills. And so on and so forth.
It used to be that a person's family doctor was able to treat severe pain. The pendulum has swung so far to the other side that those like myself can't get pain relief when we need it. Instead we're made to wait for weeks and weeks to go to a pain center. Our suffering is being ignored until the system can fit us into its schedule. And then we're being treated as addicts or potential addicts.
This is the new reality.
(Also posted in the Pain Forum: I'm Going to Be Frank About Pain)
-
Fibromyalgia
Corky, Your welcome on the pain info. It was from WebMD.I didn't reinvent the wheel. It's appropriate to bring it here rather than clicking back and forth. Easy for us to talk about the different sections.
The advent of pain management was a good thing. But they're were people, docs and patients, that abused the system. The tight controls you've seen at the pain docs office are now the standard because of that abuse. Rather than thinking they are treating you as an addict, think of them as trying to protect the majority from those that would wreak the system if they could by abusing.
Yes it's important to be as educated about your problem as possible. You will then know how well your doc is systematically evaluating you. Docs know when your educated. Some dislike it. That's okay if they are still doing their job. If they aren't ditch them fast.
A really good doc will see you as a partner in trying to solve this.Important that you start journaling. Use the pain chart. Yours will be different however. With Fibro we have so many body parts that hurt. I laugh when asked my pain level. I usually respond with "which part". The intake person laughs and generally says "I need just one number". They have one box. Right there you know that person hasn't a clue, AND the computer program was developed by clueless people.
What would be more appropriate is to be able to give a score for each body part. What that would allow is to see trends of each area. Once trends were identified, then extend that to evaluating activity that occurred just previous to the trend change(1-4 days). Much Pain & Effect or no Pain &Effect could be seen. If P&E is seen, we change the activity. If no P&E is doesn't mean that there is no reason or the info is useless. We just don't know how to use it yet. Journal. Consider at a big part of your care that will lead to an answer. It will be boring as hell and after a week or so you will want to quit it. Don't, please.
Also, journal what you are eating and type of drink. Again boring, but they're is a connection between food and food intolerances that can lead to pain. With the food journal also document how much total fluids you are drinking. Dehydration can cause pain. Just a note about alcohol it can cause pain.
Next box I will make a pain chart for a fibro person. Then the box after a diet chart.
Hugs Cory. Remind me to reread your post for the micro details. I read it in the Macro sense the first read through.
-
Lets start the chart with some abbreviations
D=date, T=time. A=activity. W=work, O=off, E=exercise. B=bed, a bed day definition is "to hurting to get out of bed". I will possible add abbrev. as it develops. MouthB=mouthbreating
If anyone wants to make suggestions , please do. Plus, this is your chart. If you can see it works better doing it a different way--DO IT
 Once the chart is done, run it off and make grid lines. Using line paper will reduce the work. Suggest again as before of using a ring binder.
Once the chart is done, run it off and make grid lines. Using line paper will reduce the work. Suggest again as before of using a ring binder.I would like to see 7 days , but the staring of the week is Monday. I would like to see how our bodies perform on two connected weekend days. Plus, for working folks an abbreviation for work and off. Back up to the top.
................D&T...A......... D&T...A........ D&T...A........ D&T...A......... D&T...A......... D&T...A......... D&T...A ..........
_score each on 0-10____________________________________________________________________________________
head
_______________________________________________________________________________________
tinnitus
_____________________________________________________________________________________
dizziness
____________________________________________________________________________________
eyes
____________________________________________________________________________________
TMJ
___________________________________________________________________________________
neck
_______________________________________________________________________________________
thoracic
_____________________________________________________________________________________
lumbar
_____________________________________________________________________________________
pelvis
____________________________________________________________________________________
shoulderR______________________________________________________________________________________
shoulder
_____________________________________________________________________________________
humerusR
_______________________________________________________________________________________
humerusL
_______________________________________________________________________________________
Larm R
_______________________________________________________________________________________
Larm L
________________________________________________________________________________________
fingerR
_______________________________________________________________________________________
fingerL
________________________________________________________________________________________
chest
________________________________________________________________________________________
abd- - |--
_______________________________________________________________________________________
hipR
__________________________________________________________________________________________
hipL
_________________________________________________________________________________________
femurR
__________________________________________________________________________________________
femurL
__________________________________________________________________________________________
LlegR
___________________________________________________________________________________________
LlegL
___________________________________________________________________________________________
footR
___________________________________________________________________________________________
footL
____________________________________________________________________________________________
pfasciaR
__________________________________________________________________________________________
pfasciaL
_________________________________________________________________________________________
Sleep
apnea
___________________________________________________________________________________________
Nose
MouthB
____________________________________________________________________________________________
Sheet
twisted
______________________________________________________________________________________________
Hair mess
twisted
_____________________________________________________________________________________________
-
Corky, had the longest most thorough post to you. Damn gone twice. Irony I was saving it b/c I get nervous with long posts being lost.
-
Corky, Now to take a micro look at your complaints. Each doc has a body part or function that they work. It's happened because of the explosion of knowledge in the last 60 years. What is a problem is integration of what's learned in the individual parts/function and how it applies to the whole body or other body parts.
" I suffer from fibromyalgia and pelvic pain. Due to vag atrophy I've had many UTIs. My PCP says that the atrophy is responsible for the pelvic pain and UTIs but she can't prescribe Vagifem due to my ER+ status. Instead she referred me to a urologist, a gyn and a pain center. I told her that my pain is often a 7 out of 10 and she recommended Tylenol. I've been at this level of pain for months with no relief. She will not prescribe opioids."
I have a vulva problem as a result of Radioactive Iodine 131 for Thyroid cancer. Get the pain doc to refer you to a Oncologist Gyn. Not that I believe you have vulvar cancer. It's b/c in my doctor traveling I've learned they know the most about the vulva. When they biopsy they have a better idea of what they are biopsing. Shouldn't be so , but that's my experience. Alternatively, a Dermatologist that ROUTINELY does vulvar exams and biopsing would be just as good. But make sure they do before wasting time seeing them.
The absolute key to the biopsy is it be examined by a Dermatopathologist. The specialize in skin and are familiar with the rating system for vulvar tissue.
If your vulvar problem is really just post menopausal atrophy, it's treated with certain drugs. If it's something else. It's treated with a different set of drugs.
On to the UTI's. Were they found on random voids for urinalysis? Or were you symptomatic i.e burning, urgency, frequency, fever, chills, systemically ill? If you haven't had the look into the bladder it would be worth it to do so, if these are frequent. It is usually done in the office. Do it at a major center. They usually have laproscopic type equipment versus they old scopes. No sedation over in ten minutes.
Frequent UTI's that have no symptoms, that are found on random voids for urinalysis have been highly debated for years(20) as to whether they should be treated. Plus, the discussion of whether the voids are inadvertently contaminated from vulva bacteria is a serious question too. Bacteria is a normal flora of the vulva. The treatment for a UTI is antibiotics. Antibiotics weaken the immune system. If a bacteria needs to be treated than let it be so. BUT if it's in it's normal habitat, it's not a good use. Basically that's been the controversy for the last 20 years.
Think I'm done for the night. Hugs
-
Sassy, the UTIs were diagnosed because of all the symptoms. Four UTIs in five months. The urologist will do a cystoscopy in a month. It's an office procedure and the handout they gave me says the actual scope part of the procedure will take 1-3 minutes, longer if a biopsy is done. It also says that the scope is the size of a pencil. Trying not to think about that!
The gyn referral is to see if there is any estrogen product that I can use at all. There is no vulvar pain or skin symptom. It is all burning and aching internally. It is pelvic pain not vulvar pain. I don't think an oncologist gyn is necessary for this. It seems that around here all the gyns are also OB docs. I would love to find one who specializes in post-menopausal women, if such a sub-specialty even exists.
The chart looks great; I will have to print it out.
-
-
Thanks Mags will get to it with the next brain discharge
Corky. The office scope is a piece of cake and you will get the results immediately, unless your doc was different than mine. Ask your Gyn doc if an Endocrine doc would run any different tests than they are running?
-
Thanks Sassy.
In the meantime, I have had an interesting week of pain. I went to a pain management clinic. No opioids recommended for fibromyalgia or pelvic pain. No matter if pain is 7/10. They recommended acupuncture and cognitive behavioral therapy. I found a community acupuncture location at a senior center. The doctor charges $10 per session for members and $15 for non-members. I've already had one session and intend to try at least two months, once per week. The sessions are in a large room, patients are all in the same room in portable lounge chairs. Since my insurance doesn't cover acupuncture this place is a Godsend.
I am actively searching for a cognitive behavioral therapist who takes my insurance.
Now, about the pain management clinic. It was in a rundown part of town. I could deal with that. But the restroom was dirty, actual dirt on the floor and the floor was sticky too. Inside the tray that was for the urine sample cup was written, "Do not urinate in tray." The waiting room smelled like cigarette smoke and perfume. I told my PCP that I don't feel comfortable in that environment and asked for a referral to other pain clinic in town. It is in a nicer part of town. Who knows if it smells or not.
BTW, the nurse practitioner that I saw at the pain clinic said, "it's not that I don't believe you're having pain BUT...."
-
CORKY OMD, sounds like a drug den, pill mill. Awful. Please, if you can start the pain record. Problem with Fibro is it's primarily Women's disease and it's still not clearly understood. Which I know you know. Meant for readers that don't know that. I haven't read Mags article yet, but she described it. there has been some success with Rituxin. OH so hope it plays out that way.
-
Sassy, I don't know about it being a pill mill. They don't give opiates at first visit, your PCP has to give a one-month bridge prescription. They count the pills in your bottle then urine test you to make sure that the concentration in urine matches number of pills missing. You must take the amount that your script says, no more or less. And then you have to carry around a letter from the center that shows an ER that you are allowed pain meds if you are in pain. I am regretting that I am in the system. I don't even get pain meds to begin with! If this new place has nothing new to offer me I may just get off this merry go round.
I read the article on Rituxin. It sounds very experimental. And as cancer patients do we really want our immune systems depressed?
-
Corky, That was my knee jerk reaction about the facility you were in. Florida was notorious for pill mills. Part of why there was a crack down nationally. Every news video that I saw when a raid was shown on TV, the pill mill was in a shady part of town. looked decrepit with people lined up outside. Views of licensed from out of state "patients". It wasn't a good time.
Haven't read the rituxan article yet, likely won't get to it till next week. Big family gathering this weekend. Shoulda been preparing before this.
-
Rituximab for chronic fatigue syndrome
Mags and Corky, Well this is encouraging. Even though the study is small, a 67% response in the Rituxin group is significant. The fact that patients remained symptom free from 8 to 44 weeks. Anyone with CFS would adore to be symptom free for any amount of time. This study also opens up many avenues of research. The researchers didn't understand the mechanism of how it worked, but they know something worked. To a researcher that's like dangling cheese in front of a mouse.
The two in the placebo group that saw improvement with one seeing long term improvement. The placebo effect shouldn't be discounted. The brain is a wonderfully intricate organ. Going to google placebo effect and see if they're any researchers that have dedicated their life's work to unravelling this. Sorry, didn't find anything. Doesn't mean it's not out there, my search didn't pull anything. However did write a short post on Placebo Effect.
Must seriously admit my eyes kept going back to the 44 weeks in the study. Anyone here with long term chronic pain will understand.
Categories
- All Categories
- 679 Advocacy and Fund-Raising
- 289 Advocacy
- 68 I've Donated to Breastcancer.org in honor of....
- Test
- 322 Walks, Runs and Fundraising Events for Breastcancer.org
- 5.6K Community Connections
- 282 Middle Age 40-60(ish) Years Old With Breast Cancer
- 53 Australians and New Zealanders Affected by Breast Cancer
- 208 Black Women or Men With Breast Cancer
- 684 Canadians Affected by Breast Cancer
- 1.5K Caring for Someone with Breast cancer
- 455 Caring for Someone with Stage IV or Mets
- 260 High Risk of Recurrence or Second Breast Cancer
- 22 International, Non-English Speakers With Breast Cancer
- 16 Latinas/Hispanics With Breast Cancer
- 189 LGBTQA+ With Breast Cancer
- 152 May Their Memory Live On
- 85 Member Matchup & Virtual Support Meetups
- 375 Members by Location
- 291 Older Than 60 Years Old With Breast Cancer
- 177 Singles With Breast Cancer
- 869 Young With Breast Cancer
- 50.4K Connecting With Others Who Have a Similar Diagnosis
- 204 Breast Cancer with Another Diagnosis or Comorbidity
- 4K DCIS (Ductal Carcinoma In Situ)
- 79 DCIS plus HER2-positive Microinvasion
- 529 Genetic Testing
- 2.2K HER2+ (Positive) Breast Cancer
- 1.5K IBC (Inflammatory Breast Cancer)
- 3.4K IDC (Invasive Ductal Carcinoma)
- 1.5K ILC (Invasive Lobular Carcinoma)
- 999 Just Diagnosed With a Recurrence or Metastasis
- 652 LCIS (Lobular Carcinoma In Situ)
- 193 Less Common Types of Breast Cancer
- 252 Male Breast Cancer
- 86 Mixed Type Breast Cancer
- 3.1K Not Diagnosed With a Recurrence or Metastases but Concerned
- 189 Palliative Therapy/Hospice Care
- 488 Second or Third Breast Cancer
- 1.2K Stage I Breast Cancer
- 313 Stage II Breast Cancer
- 3.8K Stage III Breast Cancer
- 2.5K Triple-Negative Breast Cancer
- 13.1K Day-to-Day Matters
- 132 All things COVID-19 or coronavirus
- 87 BCO Free-Cycle: Give or Trade Items Related to Breast Cancer
- 5.9K Clinical Trials, Research News, Podcasts, and Study Results
- 86 Coping with Holidays, Special Days and Anniversaries
- 828 Employment, Insurance, and Other Financial Issues
- 101 Family and Family Planning Matters
- Family Issues for Those Who Have Breast Cancer
- 26 Furry friends
- 1.8K Humor and Games
- 1.6K Mental Health: Because Cancer Doesn't Just Affect Your Breasts
- 706 Recipe Swap for Healthy Living
- 704 Recommend Your Resources
- 171 Sex & Relationship Matters
- 9 The Political Corner
- 874 Working on Your Fitness
- 4.5K Moving On & Finding Inspiration After Breast Cancer
- 394 Bonded by Breast Cancer
- 3.1K Life After Breast Cancer
- 806 Prayers and Spiritual Support
- 285 Who or What Inspires You?
- 28.7K Not Diagnosed But Concerned
- 1K Benign Breast Conditions
- 2.3K High Risk for Breast Cancer
- 18K Not Diagnosed But Worried
- 7.4K Waiting for Test Results
- 603 Site News and Announcements
- 560 Comments, Suggestions, Feature Requests
- 39 Mod Announcements, Breastcancer.org News, Blog Entries, Podcasts
- 4 Survey, Interview and Participant Requests: Need your Help!
- 61.9K Tests, Treatments & Side Effects
- 586 Alternative Medicine
- 255 Bone Health and Bone Loss
- 11.4K Breast Reconstruction
- 7.9K Chemotherapy - Before, During, and After
- 2.7K Complementary and Holistic Medicine and Treatment
- 775 Diagnosed and Waiting for Test Results
- 7.8K Hormonal Therapy - Before, During, and After
- 50 Immunotherapy - Before, During, and After
- 7.4K Just Diagnosed
- 1.4K Living Without Reconstruction After a Mastectomy
- 5.2K Lymphedema
- 3.6K Managing Side Effects of Breast Cancer and Its Treatment
- 591 Pain
- 3.9K Radiation Therapy - Before, During, and After
- 8.4K Surgery - Before, During, and After
- 109 Welcome to Breastcancer.org
- 98 Acknowledging and honoring our Community
- 11 Info & Resources for New Patients & Members From the Team
