Nerve Damage - CIPN & RIBP
Comments
-
Hi Cindy,
So glad all went well...sorry we weren't able to meet on the 18th I kind of thought that might happen based on your telling us how late your 1st meeting with Dr. Stubblefield went...can't wait to hear about test results and final plan for you to take back to Texas.
My 1st meeting went well, I liked him too...he changed my pain medication and I was to have MRI of brachial plexus on Saturday 8/27 but we had to reschedule to 9/12, same date I'm already scheduled for my OT evaluation.
We were evacuated from Long Beach Island on 8/25 and with Manhattan closing mass transit and bridges due to Hurricane Irene, we were afraid we'd be stuck there so we changed the appointment.
That storm was looking a lot worse as we made our way home to Syracuse...thankfully, it was down-graded but sadly it was done after our decision to leave had to be made.
Stay well, await your next up-date, Pat
-
My reply of today was to post under Cindy's third installment of 8/24/11, don't know why it posted under her 1st blog entry from earlier this year.
-
So strange...all have been in response to third installment!
-
I have the p.n. mostly in my feet..I have had a real difficulty with balance..has anyone
had a therapy that helps with that?? I do take Lyrica so I can at least use my feet without
pain
-
SoCalLisa, have you tried Tai-chi? It is really good for balance. I started classes a couple months ago, and hadn't been for a few weeks because of hectic schedule, and have found I am much more unstable than when I was doing the classes. I hope to get back to them soon. It is very gentle movement, but very focused, and the instructor said it is very good for CIPN - he says he has worked with several people with this problem.
-
thanks Linda..any luck with physical therapies?
-
MSKCC Rehab - 4th Installment
It's been a couple weeks since I've left my new friends at Dr Stubblefield's Cancer Rehab Center. I was able to speak with Dr Stubblefield on the morning prior to leaving NYC. He talked to me about the MRIs I had earlier in the week. The total spine MRI showed no additional cancer or tumor activity. I do have moderate to severe stenosis at L2-L3 and severe stenosis at L3-L4. This is what affects my lower legs/feet/toes with weakness, pain and numbness/tingling. The MRI of my Brachial Plexus did not show any additional cancer or tumor activity. It did show that the bottom 3rd portion (nerves leading to the hand/fingers) has been severely burned/damaged by radiation. The middle portion (nerves leading to the forearm/wrist) have also been severely burned/damaged by radiation. The upper portion (nerves leading to the shoulder/upper arm) has been burned/damaged, but not severely. From the elbow to fingers will continue to get worse with pain, numbness, tingling, and muscle atrophy. Eventually becoming nothing more than a dangling appendage. Time frame is an unknown factor. The upper arm, should potentially remain stronger, allowing movement to some degree. It's not the best of news, but at least confirms all that has been occurring over the years, and more so over the past 12 months. Dr Stubblefield told me that my Brachial Plexus radiation damage was the worst he has yet to see... Overall radiation fibrosis throughout the neck and chest areas was also abundant. He said that my individual case shows just how radiation treatments can damage. In particular, the Hodgkins mantle treatments of the 80's, followed by Breast Cancer overlapping radiation. He said that he is going to change his presentation and related MRI slides at his upcoming conference to use my case, because it clearly shows the long term affects of the damage caused by the radiation. He told me that i am an incredibly strong woman, for he understands the results on every day life of this type of damage. He said to be able to do as much as I force myself to do is amazing in itself. This somewhat embarrassed me, and at the same time gave me more strength. I have always done what I have to do to endure and hang onto quality of life. The same as we all do. It's never ever been easy as all of you who have had these same symptoms well know. It felt good because finally, a medical professional who actually knows what the hell has happened, and understands what the hell we actually have, and doesn't look at me with that "deer in the headlights I don't know what to tell you" look. He also reached out to my oncologist here in TX to discuss. She in turn told him she will discuss with her radiology partners. Going forward, the more they understand the long term effects of overlapping radiation fields for patients with prior mantle radiation, the more consideration they can give to the individualized treatment plan. And the more they can give to the patient for combined Dr/patient decisions on their treatment plan. I was at my oncologist this week for my 5th year "cancer-versary" from end of treatments. November 17th is my 6th year from diagnosis mark. We talked specifically about the findings of my MSKCC visit, and her discussion with Dr Stubblefield. She was grateful for his call and indicated the new information was beneficial for her and the radiologist for treatments on patients with prior Hodgkins radiation. YAY!! Finally, recognition from the oncologist world! That alone is a huge leap in the right direction.
By the way, my overall visit with the oncologist was good! No obvious signs of recurrence.... A little lab work, and I was dismissed for 1 year! That's a HUGE step!
Now, I continue with the PT/OT plan established by the MSKCC Rehab group. I still have, and will continue to have, the intense nerve pain, and constant paresthesia 24/7.... That does not go away, or get better - no magic pill or treatment. I totally get the severity of my condition, and know it can't be fixed.
The entire journey to MSKCC was well worth the time, cost, EMG pain, and exhaustion endured. The last day there, I hugged Dr Stubblefield, and cried. Same thing with the PT/OT staff.
My anticipated results were - and the RESULTS
1. A clear understanding of what damage has occurred - CHECK
2. What to expect going forward. - CHECK
3. An actual plan of action - CHECK.
4. Physical therapy to help with range of motion. - CHECK
5. Occupational Therapy to help with day to day life adjustments beyond what I've taught myself. - CHECK
6. Pain/paresthesia relief. - UNFORTUNATELY NO
7. A better outlook on quality of life. - CHECK
Overall, SUCCESS!
Stay Strong,
Cindy -
Cindy, thanks for your update. I am so sorry to hear the long-term prognosis is not so great for pain and function, but you are an absolutely wonderful and strong woman to stick with this and share the information to help prevent (hopefully) the same condition in others. Your positive can-do attitude is encouraging to me and others. I have shared a lot with my MO about my issues, anger, function, fear, etc., and she said she was actually grateful that I felt comfortable enough to share these thoughts with her. She truly cares about what happens to all of her patients, and she learns from each of us to help the next ones. I guess that's sort of what our life is about: helping others through love, and not the anger that I have had for so long. I am turning lose of that anger more every day, learning to accept a little (still struggle with it a lot some days). Blessings to you,
Liinda
-
Hi Cindy,
I echo Linda's comments and want to add how great it's been to follow your incredibly well-documented story. Your detailed account has been key to understanding your situation. Myself and others have a starting point for comparison regarding our own personal issues.
I have excruciating nerve pain and paralysis in my right hand, it feels like it starts in my fingernails and proceeds through my hand to wrist and now is going up my forearm to elbow. My hand is deformed with painful swan neck deformity most notable in the three middle fingers. I have limited gripping ability between the thumb and index finger, otherwise not much left in my right dominant hand.
It's taken time, many prayers, the support of family/friends and lots of internal struggle to overcome the anger, to find the courage to accept that I have lost the use of my right hand/arm and need to find a way to go forward with my life.
I 've never been a pessimistic person. I've always been an optimistic, positive person with a zest for life and a plan for my future, so this has truly thrown a 'monkey wrench in my life' as my dear departed father might say, So, yes, I have and will make whatever changes are necessary to go forward!
I have an appointment with OT and to do the MRI of my brachial plexus on 9/12/11 at MSKCC. From your note, and based on my symptoms, if no cancer, I can assume I too have may have damage to the lower and middle sections of the brachial plexus.
I love Dr. Stubblefield too and am so impressed he has decided to use your case in his presentation. It should do so much to get the word out to the medical profession. You should be very proud of yourself for being one of the early case studies to move our plight to front and center!
I hope and trust from this effort prevention of the problem will become foremost, with perhaps ways to effectively treat the nerve pain next, and maybe at some time in the future even finding a way to fix the nerves of those who have suffered permanent damage.
So, thank-you Cindy for your immense contribution to our cause, I am deeply indebted to you. And, I am encouraged and anxious to know my own results down the road.
I plan to continue as you have done with a report on my findings as soon as they become available. May God bless you Cindy and keep you strong.
Sincerely yours, Pat
-
Thank you Cindy for all the updates. Pat any results from your workup with Dr. Stubberfield? I so hope that the oncology community starts to understand the severity of our RIBP/CIPN and at least validates new patients with these symptoms. I am so frustrated with being seen as the oddball because "no other patient has had this".
-
OK, so I'm finally getting a chance to update my story from my last entry of 9/8/11.
I had the MRI of the brachial plexus 9/12 - it was normal, no cancer - Dr. Stubblefield wanted it read by an MD who usually did his MRI - over a week went by due to Dr. Stubblefield's vacation when he called to say, on second look, there were mild changes to the lower and middle sections of the brachial plexus consistent with RIBP.
He didn't understand why my symptoms/pain were so severe, yet findings on MRI were fairly normal. I had called him twice to up my medications, he has inched up the strength of the Fentanyl patches.
My OT evaluation went well, the therapist gave me several modalities to help my hand, she felt with hard work and by using a therapist with a CHT designation, that is a Certified Hand Therapist, I may be able to reverse the swan's neck and regain the use of my fingers, and hand.
I've been seeing Kathy Rake, CHT two times per week for about 5 weeks, and I do see improvement, but it's extremely painful, slow-going work. It took me over 1 year to get here, I expect it will take at least that time to get it back.
I saw Dr. Stubblefield on 10/24, as a follow-up, he performed an EMG also while I was there. I think he likes all tests done or repeated by his group to verify the findings. At any rate, though painful, it was not really a problem to do again.
When I got home I clarified a few things vis email with Dr. Stubblefield:
1) My diagnosis is RIBP
2) It affects the use of my median and ulner nerves, they are not functioning, or not charging the muscles correctly, which causes the problems with my fingers, hand and wrist. These nerves come out of the lower and middle plexus, which suffered radiation damage.
3) With the lower and middle plexus involved, I will experience most involvement in the hand, forearm and triceps areas. My deltoid and biceps are good and hopefully will stay that way.
4) My pain is still not under control even though Dr. Stubblefield increased to 100mg Fentanyl patch, every 48 hours, with Oxycodone 5mg for breakthrough pain, maximum 12 per day. I will need to call him again for adjustment again.
My pain is absolutely excruciating, I don't understand why it cannot be controlled, the only relief I get is lying down. I'm going to ask him to explore that further. Seems there should be an answer related to what changes in my body when I lie down that eliminaates the pain?
If anyone knows the answer or I find one, I'll update my status here. Thank-you to all for your support, it's more appreciated than you'll ever know, sincerely yours, Pat
-
PS: In addition to the medication listed above, I take 3000mg of Neurontin (Gabbepetin) per day, and an occasional 5mg of Xanax (Alprazolam) for anxiety (rarely used, can't even remember last time).
-
Thanks Pat for your update! I hate that you have so much discomfort and break through pain instances. I'm glad you can get some relief from lying down, and at least have some of the edge taken off by the pain meds. I wish I could endure narcotics to at least get some rest - but they just don't stay in my body, or allow anything else to remain in my stomach... I have to choose the pain alone, over the pain combined with vomiting... I wish TX had medical marijuana!
 Dr. Stubblefield is indeed a hero to many survivors. We need many more doctors, of his specialty, worldwide.
Dr. Stubblefield is indeed a hero to many survivors. We need many more doctors, of his specialty, worldwide.
Stay Strong,
Cindy -
Wanted to share some YouTube video posted by Memorial Sloan Kettering Cancer Center, featuring Dr Michael Stubblefield. He is describing Radiation Induced Fibrosis, and Radiation Induced Brachial Plexopathy issues for Hodgkins Disease, Head & Neck Cancers, Breast Cancers, and Sarcoma survivors. Very well done - you'll find these to be easy to understand. Dr Stubblefield is who I went to specifically see in NYC at MSKCC in August 2011. My previous installments in this forum were focused on that 2 week visit with him and his PT/OT staff. This is good stuff!
 http://www.youtube.com/watch?v=xumJojH94Ts&feature=youtube_gdata_player
http://www.youtube.com/watch?v=xumJojH94Ts&feature=youtube_gdata_player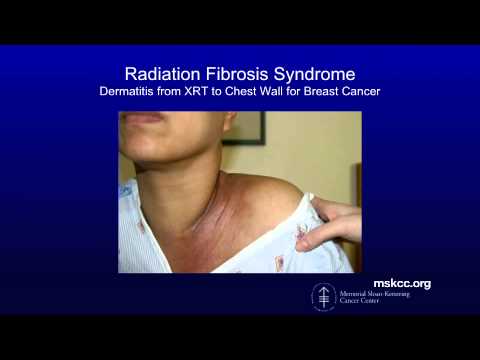 http://www.youtube.com/watch?v=LvZJKNtNXXc&feature=youtube_gdata_player
http://www.youtube.com/watch?v=LvZJKNtNXXc&feature=youtube_gdata_player http://www.youtube.com/watch?v=cp5PGCUYRdE&feature=youtube_gdata_player
http://www.youtube.com/watch?v=cp5PGCUYRdE&feature=youtube_gdata_player http://www.youtube.com/watch?v=dczzQxAaLYQ&feature=youtube_gdata_player
http://www.youtube.com/watch?v=dczzQxAaLYQ&feature=youtube_gdata_player
Stay Strong,
Cindy -
Hello Everyone,
I wondered if anyone is a Nurses with CIPN? I am a Nurse and I have CIPN and due to the numbess,tingling and needle prick sensatios I endure I am limited. I recently was asked by my employer to come back to work with my limitations that was accompanied by a MD note. Once I started working the position my employer told me about never started.My employer informed me they would require me to do patient care visiting patients in their homes. I expalined to my employer my limitations as discussed prior to me returning back to work did not include patient care due to the neuropathy.My employer stated I could use an automatic cuff (instead of the cuff that require me to manually inflate the cuff which requires dexterity I am unable to perform at this time).I tried to explain to my employer it is more than inflating a b/p cuff my fingers are numb I cannot feel a pulse (employer response: the patient will not have a pulse taken on that visit) I can not stand (response from employer we will take a nurse poll of the patient houses you would have to stand in).Although my Physican note clearly states my limitations my employer seems to ignore what my limitations are.
At this point I decided my employer either does not believe the limitations i have with my neuropathy or does not care. I did not try to go on with the many scenarios of how my neuropathy interferes with caring for a patient . I feel frustrated I know my employer probably looks at me and does not see a person that endures pain and discomfort. I do not visibly show discomfort nor do I complain.I have always been a person to try to endure.This neuropathy is a different animal I told my husband when I cared for patients prior to my neuropathy at times depending on wear they lived I had to park my car and walk a block or more depending on the location.Then there are the patients who depending on what care you have to give may or may not have buttons or zippers not to mention some patients due to their condition you have to stand and bend to perform care. All of which was fine before this happened to me.There are so many more scenarios that my neuropathy would interfere taking care of patients.
I have always been a "worker bee" never without a job sometimes two at a time.To be in a situation where you a limited is very frustrating. To get through chemo and mastectomy surgery and all the stress that comes with it to have to now endure my employer adding more stress to me seems so unfair.I wish there was more education so employers or those who think patients with CIPN may not look like they are in pain or verbalize they are in pain does not lessen the fact we are.If they could feel how my feet burn when i am at work from just walking down the hallway but I endure because I tell myself I will sit down and relax my feet when I return to my desk.Or when I have to walk to the next level for something by the time I return upstairs and return to my desk my feet are on fire and throbbing.I told my husband I know i have to stop myself before walking but at the time a rationalize with myself and say"it is a short walk"Or "It is only down the hall" Only down the hall is like forever for me right now with this neuropathy.
I know not helping myself and I have to stop before walking which is hard but it is the natural thing to do but not for my condition.The stress of knowing what my employer wants me to do does not help.When I get home after work my feet burn like no tomorrow and my hands are now starting to catch up with my feet.I do some typing at work I am now using a pencil to type on the keyboard and that helps a little.
I wondered if there are any nurses that are having the same trouble I am having at work? if so I would love to hear from you.And if there is anyone that knows a nurse with my same issue.I know on paper my physician will inform my employer I am not able to care for patients at this time it is the stressful environment I am not looking forward to everyday. Any advice?
-
Jen, I'm not a nurse, but I do know that it's possible to appeal to the U.S.Equal Employment Opportunity Commission (EEOC) on the basis of a disability that requires reasonable accomodation in the workplace. Their filing form is not difficult to fill out, and it's good to have someone on your side as you deal with your employer.
http://www.eeoc.gov/employees/charge.cfmOf course that requires you to be willing to accept the designation of "disability" for the neuropathy, and perhaps you're not ready to do that yet. If not, it's a goal to keep in mind as you work through the grieving process that goes with this.
 Grief takes time, for sure, but the EEOC can make it easier.
Grief takes time, for sure, but the EEOC can make it easier.Just a thought. Be well!
Binney -
Jen, I am also not a nurse, but know the frustrations of not being able to perform in a chosen career due to the neuropathy. One thing I have tried to do more of is to articulate what I CAN do rather than what I CANNOT do. This can serve as a discussion point with your physician, who can then write more specific guidelines for your employer, and you can use this to discuss with your employer options that will make the best use of your knowledge but will not harm you (or patients, for that matter!!). I assume you are a floor or ICU or special unit nurse who needs to be on your feet most of the time. There are positions in case management, managed care, making sure providers are paid, teaching, working in a poison control center, phone triage and nurse information lines, etc. Mostly, you need to look at what you can do and what you LIKE to do. That's not so easy when you are grieving the loss of a previously healthy body that would let you perform all the activities of your chosen career, but it does help employers and others to help you. Rather than giving them a menu of what you cannot do, give them a menu of what you CAN do, and see if they can work with that a little better. Prayers for peace and healing - this is a tough road. PM me if you want to toss some more ideas around. My younger sister is a nurse who no longer does bedside nursing.
-
My arm is shrinking! I've noticed muscle wasting in my r arm. Nerve damage? Onco saw it, not worried, called BS nurse - never heard of it. My GP measured it and will check again in 6 months.
It is on my affected side. Thoughts? -
Cindy and all,
I actually didn't have breast cancer butt have gleaned much information from various breast cancer sites. Cindy has provided a wealth of information. I was actually diagnosed with a soft tissue sarcoma deep in the scapular muscles in September 2010. I received 25 rounds of radiation which wasn't bad until the very end when I discovered the skin in my armpit was weeping. Then it was three weeks of "heck" waiting for it to heal. I had surgery in December 2010 where they removed the muscles over the right scapula, part of the deltoid and part of the lat muscle. I had limb sparing surgery because there was a possibility that the cancer had infiltrated the humerous. So, a partial shoulder replacement was done leaving me with no rotator cuff. Two days later a muscle flap reconstruction was performed to try to provide protection to the scapula. All went well, I was knitting within two weeks and started physical therapy.
At the end of January I started chemotherapy which set my physical therapy progress back. I finished chemo, along with 6 blood transfusions and 2 platlet transfusions in April. As soon as I recovered I started PT again. I noticed some numbness in the fingers of my right hand but it was chalked up to neuropathy. I went back to work, got my writing back up to speed, could keyboard as fast and accurate as ever and continued to knit. I could even put my car into gear with my right hand. In July I went on vacation and noticed that my fingers were fumbly trying to knit. By the end of August I could no longer write with my right hand and had resorted to one handed typing. The physical therapist didn't know what to do for me because I could no longer hold onto the equipment.
I had an EMG, MRI, saw the neurologist,radiation oncologist, oncologist and surgeon. RIBP was the consensus. Right now I am in the midst of hyperbaric oxygen treatment which may or may not help. I saw Cindy's posts about Dr. Stubblefield and decided to give him a shout. I just got back from seeing him. he said exactly what I expected. There is nothing that can be done to reverse the damage. That will either happen on it's own or it won't. He prescribed Lyrica to replace the Neurontin and gave me prescriptions for PT, OT and lymphedema therapy. I haven't had issues with lymphedema, but he saw me at my absolute worse. I'd been in NYC for two days before I saw him and had been walking around a lot. When my arm hangs down for too long, like when walking my palm will swell.
So, I'm off to find a therapist here that can think outside the box when dealing with me. I have no good shoulder movement and can't hang onto an elliptical or arm bike. I go back to Dr. Stubblefield in June. Hopefully I can get better ratings than -4 next time.
I don't have the pain most talk about, or I just don't recognize it as pain. I have a high tolerance. I am uncomfortable and frustrated and do have the electrical feelings in my fingers and a vise-like feeling. Until about three weeks ago I could extend my fingers voluntarily, but I have lost that ability.
This just sucks, but I have my arm. Many years ago that wouldn't have been an option. And my handle, Tubthumpin? It's a song; I get knocked down, but I get up again ....."
Lori
-
Lori, welcome! Have you found the RIBP thread in the "Lymphedema" section of the discussion boards here? It's near the top of that forum. There's also an RIBP information page that was developed by many of the women here at bc.org who have RIBP. It's here:
http://www.stepup-speakout.org/Radiation_Induced_Brachial_plexopathy.htmYour music choice (and your spirit!) is an inspiration! Be well,
Binney -
It's been a long time since I've posted anything specific about myself, or to anyone else, on any of the forums... Other than various articles of interest to share.
Getting back into it has been difficult emotionally for me - both my parents passed away last year. First my Mom, in July, followed in two very short months by my Dad, in September. This was more difficult than I had ever imagined it would be. My Dad would love to read anything I wrote. He would read them out loud to my Mom, as she could no longer see. Dad would share them with anyone he would encounter. He always told me he was proud of me. So, whenever I start to write, I think of that. Up until now, that was holding me back. No longer can it be my excuse. Instead, it will fuel me.
Jen - how are things going now with your employer? Any success in getting them to understand how difficult it is for you to perform your day to day routine? I was fortunate with my employer and management regarding my special needs. That actually lasted about a year... Changes in desk setup, changes in work hours, working mostly from home. I have now gone on full disability. I too was a "worker bee" pushing through the days and evenings. Unfortunately, it began to take me 12 hours to complete 8 hours of work. The stress becoming more and more concerning. It's taken me several months to get used to not forcing myself beyond capabilities. I have a new stress, and that is $. Disability only nets about 50% of what I had been able to earn. Sad. But we are working through it, making changes, and making it work.
Enduring the nerve pain, tingling, electricity, numbness, weakness and overall discomfort is what we do, 24/7. It is down right miserable. It sucks. We try hard to not be as visibly miserable to others, as we want them not to suffer along with us. We want them to want to be close to us. We want to be able to do the things we loved. So we find a way. Being miserable and defeated does not invite many people to remain close. We want to be happy. For the most part we are. We want to be "normal" again - like we were before. That's not gonna happen. I understand that, but I don't like it. As none of us do. The Internet has given us many avenues to obtain information, and very importantly the ability to find others who are enduring the same miserable symptoms as we do. Wow... We are not alone! We have others we can vent to who do "get it"!! I can't imagine how difficult this could have been for people 25 years ago.
I would love if we could somehow share our new found disabilities and physical feelings with our medical care givers, employers, insurance companies, our government, research grant holders, family, friends, etc., who truly don't understand how this type of nerve damage feels. If we could share exactly what we are feeling with them, so they could have a true sense of how this affects us, then they would "get it". Just share those physical feelings with them like a Vulcan "mind meld" for a short time. Brilliant!!
Lori - i hope you are doing well. I am sorry you too are a victim of RIBP. It shows that radiation damage is not only affecting BC or Hodgkins Lymphoma survivors. And it adds to the many of us who are looking for help. Looking for answers. Looking for changes for future treatments. There must be some way the Brachial Plexus can be preserved throughout radiation treatments. There must be some way to ensure our lives are ridden of the cancer, AND ensure the life saved, can survive with the highest quality possible.
The more collective voices we have, the louder we become. The louder we become, the more opportunity to be heard.
Dr Stubblefield is a giant of a man. He, is helping us have a voice. He is sharing much needed knowledge to the medical field world wide. My Oncologist's PA talked with me the other day. We discussed my issues and damage from the chemo and radiation. She, recognizes the need for continued care of the survivor. She told me that this need is finally escalating. And that she would love to be a part of it. Is that not the best news!! Think about it, a clinic or Dr we could go to after the Oncologist turns us loose as a survivor. Someone who understands a "cold" for us is different then all other patients coming into a primary care physician. Someone who is extremely knowledgable of cancer survivor needs. Incredible! I believe we are making headway! :)
Binny - I hope you too are doing well.... I think about you often.
Pat - has the change in meds help your day to day pain? We haven't chatted in quite awhile. Are you going back to MSKCC - Dr Stubblefield any time soon? It's fortunate that your sister is relatively close there in NJ to visit at the same time. :)
I was asked to write a short story for the Memorial Sloan-Kettering Bridges magazine, regarding my visit to the Rehab Center for survivors in August 2011. Here it is, in the Bridges - Spring 2012 edition.... Page 7, titled Surviving Survivorship. :)
http://www.mskcc.org/cancer-care/survivorship/newsletter-survivors
I hope everyone is doing well, and fighting the fight.
Stay Strong,
Cindy -
Here's something we can do to help get some attention..... LIVESTRONG cancer survey. Also, check out OVAC - One Voice Against Cancer. http://www.ovaconline.org/ They take the information we share via surveys and such, and use it to present to Congress for government funding of Cancer Research and Patient Aide. They are an advocate for us all in the US. Here is the link to the survey http://www.livestrong.org/cancersurvey. Stay Strong, Cindy.
-
Hey y'all.... I finally started a blog.... Long overdue. Please take a look! Thanks! http://survivingsurvivorship.blogspot.com/
-
Radiation damage, I wish I would have known!
-
Iam totally confused, I have read some threads & not sure if the pain I have is CIPN. Started about 6 mths after last chemo treatment, in my left arm. Feels prickly, stinging, heavy, fingers are numb. Sometimes its excruciating pain & other times its managable but there is pain ALL the time. Some times if I move it the wrong way I see stars it hurts so bad. I dont sleep thru the night it hurts so bad, pain meds dont work (I have taken 2 vicadin & didn't work). I seen my Onc who didnt give me any answers & said to use aspercream (didnt work) & my surgeon. He said because I dont have full range of my arm (where nodes were removed) that is the reason for the pain. Told me I needed to start exercising or go to PT. I cant imagine this never going away & living with this. I expected once chemo was over Iwould bounce right back, I guess I was delusional
-
Hi Michelle! I'm sorry to read about your pain. That kinda pain sucks indeed! I had a double mastectomy and nodes removed from the right armpit area. My left arm was similar in pain to what you are describing. It has taken many PT and massage therapies to help stretch that area to where I don't get that type of severe pain in it. And it was indeed from the surgery and resulting scar tissue. I would take the doc up on a prescription for PT to help release that binding tissue. I think it would help you feel much better.
 Give it time as it is hard to get that tissue to loosen up again. My RIBP came from excessive radiation for two cancers. Same with the CIPN from taxotere in the 80's and again in '06. There are specific tests, EMGs, to diagnose RIBP & CIPN. I hope that helps you..... hugs your way sister!!
Give it time as it is hard to get that tissue to loosen up again. My RIBP came from excessive radiation for two cancers. Same with the CIPN from taxotere in the 80's and again in '06. There are specific tests, EMGs, to diagnose RIBP & CIPN. I hope that helps you..... hugs your way sister!! 
-
Michelle, the pain you are describing is most likely NOT CIPN - that usually affects fingers and toes and is usually both sides. Because your pain is in the ALND arm, it could be due to radiation, but it could also be scarring, cording, or even LE. Seeing a PT who can do myofascial release, and who is also certified in LE therapy would be your best bet. He/she can measure your arm to be sure it is not LE, and work with you on scar release. One of the several neuropathic pains I am dealing with is similar to what you are describing, and the myofascial release has been a godsend. I am following that up with movements such as qi qong and yoga, and the more I keep the area moving/gliding, the better I do. I still feel the pain and tightness, but it is better. I also had cording, which the PT worked on and that completely resolved the issue.
However, if it is due to radiation damage, that is a whole different issue, and as Cindy said above, getting the right diagnosis with the right studies can save you lots of angst in the long run. If your MO and BS can't help you, find a palliative care specialist or pain management specialist to help sort it out. These are underutilized resources!
Best wishes and gentle hugs. -
Thank you Cincerely & Linda, I am definately going to have to call my DR to probably start up PT because I just cant take it anymore, tingling has started in my feet now!!!!! Linda this may sound stupid but......what is LE?
-
LE = lymphedema. Good luck with the PT. When did you finish chemo? There is a phenomenon called "coasting" where the neuropathy seems to get better, then gets worse, even months after chemo. I think there is testing that can help figure it out, but my MO and neurologist didn't do any testing at all - they just based the diagnosis on the timeline because it was pretty clear-cut in my case, but I think it is possible to figure it out with those cases that don't follow the textbook description.
I also found that fatigue can worsen the pain, so getting rest is really really really important!
Best wishes. -
Wow, I need to do more research, as I have learned so much here. I didn't really know about CIPN or RIBP. I had AC twice also, once in 2003 and the again in 2011, I also had taxol in 2003 and abraxane/avastin in 2011. I had radiation in 2003 and then on the opposite side in 2011 with overlap. My last chemo was Oct. 2011 and last Radiation was March 2012. Just had a hysterectomy Oct. 2012. I had to quit my job recently because i was miserable. My arms would tire, my legs, back, calves hurt and I don't sleep. I have to rest after doing about 20-30 minutes of housework, so it takes me a long time to get anything done. My hands and toes are tingly and numb, and the numbness spreads up my calces sometimes. I am extremely sore in the morning, it takes me a few hours to really get going and to feel half way normal. I keep waiting to bounce back like I did after my first diagnoses but it is just not happening. My docs just say to exercise more, I do walk every day about 30 minutes but I don't seem to be getting stronger. I drop things, am afraid to go down stairs and do it very slowly because I might trip from my numb feet. Wow, do I ever sound like a whiner, but I am so glad there might be a medical reason for all this. I feel like everyone just thinks I am being lazy, but that is not the case, I just can not physically do what I want to. I am tired of being in pain and just don't know what to do about it. Oh, scans and such have been clear of cancer, most recent one was in AUgust/September. Tired of getting scans too, so stressful.
Anyways, thank you for this information, I am going to look some of it up now...
Categories
- All Categories
- 679 Advocacy and Fund-Raising
- 289 Advocacy
- 68 I've Donated to Breastcancer.org in honor of....
- Test
- 322 Walks, Runs and Fundraising Events for Breastcancer.org
- 5.6K Community Connections
- 282 Middle Age 40-60(ish) Years Old With Breast Cancer
- 53 Australians and New Zealanders Affected by Breast Cancer
- 208 Black Women or Men With Breast Cancer
- 684 Canadians Affected by Breast Cancer
- 1.5K Caring for Someone with Breast cancer
- 455 Caring for Someone with Stage IV or Mets
- 260 High Risk of Recurrence or Second Breast Cancer
- 22 International, Non-English Speakers With Breast Cancer
- 16 Latinas/Hispanics With Breast Cancer
- 189 LGBTQA+ With Breast Cancer
- 152 May Their Memory Live On
- 85 Member Matchup & Virtual Support Meetups
- 375 Members by Location
- 291 Older Than 60 Years Old With Breast Cancer
- 177 Singles With Breast Cancer
- 869 Young With Breast Cancer
- 50.4K Connecting With Others Who Have a Similar Diagnosis
- 204 Breast Cancer with Another Diagnosis or Comorbidity
- 4K DCIS (Ductal Carcinoma In Situ)
- 79 DCIS plus HER2-positive Microinvasion
- 529 Genetic Testing
- 2.2K HER2+ (Positive) Breast Cancer
- 1.5K IBC (Inflammatory Breast Cancer)
- 3.4K IDC (Invasive Ductal Carcinoma)
- 1.5K ILC (Invasive Lobular Carcinoma)
- 999 Just Diagnosed With a Recurrence or Metastasis
- 652 LCIS (Lobular Carcinoma In Situ)
- 193 Less Common Types of Breast Cancer
- 252 Male Breast Cancer
- 86 Mixed Type Breast Cancer
- 3.1K Not Diagnosed With a Recurrence or Metastases but Concerned
- 189 Palliative Therapy/Hospice Care
- 488 Second or Third Breast Cancer
- 1.2K Stage I Breast Cancer
- 313 Stage II Breast Cancer
- 3.8K Stage III Breast Cancer
- 2.5K Triple-Negative Breast Cancer
- 13.1K Day-to-Day Matters
- 132 All things COVID-19 or coronavirus
- 87 BCO Free-Cycle: Give or Trade Items Related to Breast Cancer
- 5.9K Clinical Trials, Research News, Podcasts, and Study Results
- 86 Coping with Holidays, Special Days and Anniversaries
- 828 Employment, Insurance, and Other Financial Issues
- 101 Family and Family Planning Matters
- Family Issues for Those Who Have Breast Cancer
- 26 Furry friends
- 1.8K Humor and Games
- 1.6K Mental Health: Because Cancer Doesn't Just Affect Your Breasts
- 706 Recipe Swap for Healthy Living
- 704 Recommend Your Resources
- 171 Sex & Relationship Matters
- 9 The Political Corner
- 874 Working on Your Fitness
- 4.5K Moving On & Finding Inspiration After Breast Cancer
- 394 Bonded by Breast Cancer
- 3.1K Life After Breast Cancer
- 806 Prayers and Spiritual Support
- 285 Who or What Inspires You?
- 28.7K Not Diagnosed But Concerned
- 1K Benign Breast Conditions
- 2.3K High Risk for Breast Cancer
- 18K Not Diagnosed But Worried
- 7.4K Waiting for Test Results
- 603 Site News and Announcements
- 560 Comments, Suggestions, Feature Requests
- 39 Mod Announcements, Breastcancer.org News, Blog Entries, Podcasts
- 4 Survey, Interview and Participant Requests: Need your Help!
- 61.9K Tests, Treatments & Side Effects
- 586 Alternative Medicine
- 255 Bone Health and Bone Loss
- 11.4K Breast Reconstruction
- 7.9K Chemotherapy - Before, During, and After
- 2.7K Complementary and Holistic Medicine and Treatment
- 775 Diagnosed and Waiting for Test Results
- 7.8K Hormonal Therapy - Before, During, and After
- 50 Immunotherapy - Before, During, and After
- 7.4K Just Diagnosed
- 1.4K Living Without Reconstruction After a Mastectomy
- 5.2K Lymphedema
- 3.6K Managing Side Effects of Breast Cancer and Its Treatment
- 591 Pain
- 3.9K Radiation Therapy - Before, During, and After
- 8.4K Surgery - Before, During, and After
- 109 Welcome to Breastcancer.org
- 98 Acknowledging and honoring our Community
- 11 Info & Resources for New Patients & Members From the Team